New gene therapy shows promise for treating age related macular degeneration
Researchers from Trinity College Dublin have developed a new gene therapy approach that shows promise for treating the dry form of age related macular degeneration (AMD)—a progressive eye disease that affects up to 10% of adults over 65 years of age and is a leading cause of severe vision impairment and blindness in this age group.
Dry AMD cases represent about 85–90% of all AMD cases and there are no treatments available to treat or prevent disease progression, underlining the need for developing treatment options for this debilitating disease. In adults, many diseases of aging have been found to have defects of mitochondrial function, including AMD.
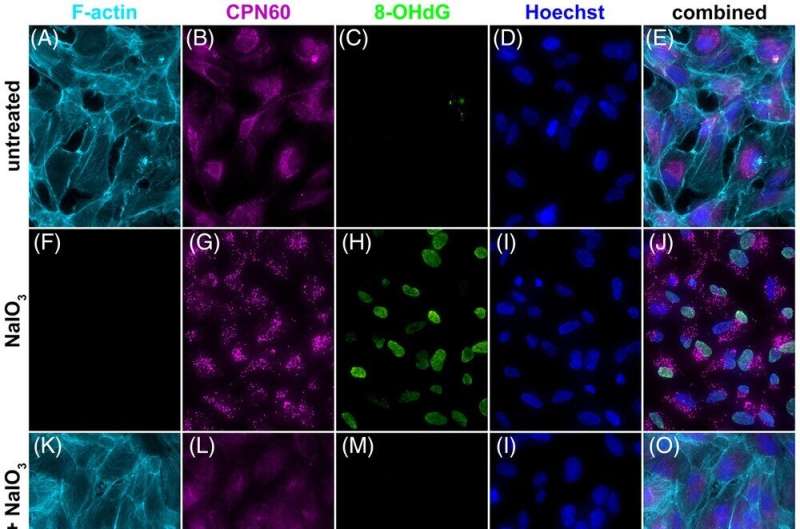
The team, in Trinity's School of Genetics and Microbiology, have developed a new gene therapy (ophNdi1) that is the first of its kind to directly target mitochondrial function in cells that are malfunctioning in AMD. Mitochondria are known as the "powerhouses" of the cell because they manage the production of energy but their performance dips greatly in dry AMD and this is linked to a deterioration in sight.
The new gene therapy cleverly uses a virus to access the cells that are suffering and deliver the code needed to give the failing mitochondria a lifeline, enabling them to generate extra energy and continue to function in supporting vision. The therapy has shown benefit in multiple models of dry AMD, offering hope that it could one day progress to a treatment that could help millions across the globe.
Professor Jane Farrar, senior author, said, "Critically, this study provides the first evidence in models that directly modulating bioenergetics in eye cells can provide benefit and improve visual function in dry AMD. In doing so, the study highlights the energy powerhouses of the cell, mitochondria, as key targets for dry AMD."
Dr. Sophia Millington-Ward, first author and research fellow in Trinity's School of Genetics and Microbiology, said, "The novel gene therapy targeting cellular energy, or mitochondrial function, that we explored for dry AMD consistently provided benefit in the model systems tested. Many retinal cells, essential for vision, require particularly high levels of energy compared to most other cells, which makes them particularly vulnerable to mitochondrial dysfunction. The therapy we are developing directly targets mitochondrial function and increases energy production levels in the retina, which leads to better visual function in disease models of dry AMD.
"Although there is further work to be done before this could be made available as a treatment for patients, the results give us hope that we are getting closer to a solution to this challenging, debilitating condition."
The study has just been published in Clinical and Translational Medicine.
More information: Sophia Millington‐Ward et al, AAV‐mediated gene therapy improving mitochondrial function provides benefit in age‐related macular degeneration models, Clinical and Translational Medicine (2022). DOI: 10.1002/ctm2.952



















