Converging epidemics: COVID-19 lockdown may have accelerated HIV transmission in some at-risk populations
A new study led by researchers at UBC and the BC Center for Excellence in HIV/AIDS (BC-CfE) is shedding light on how COVID-19 pandemic restrictions impacted another long-standing public health threat—HIV.
The study, published in The Lancet Regional Health—Americas, examined HIV transmission during British Columbia's initial COVID-19 lockdown (March 22 to May 20, 2020) when stringent public health measures reduced social interactions and curtailed access to critical health services. The researchers looked at the impact of these restrictions on populations at risk of acquiring HIV, including people who use drugs (PWUD) and men who have sex with men (MSM).
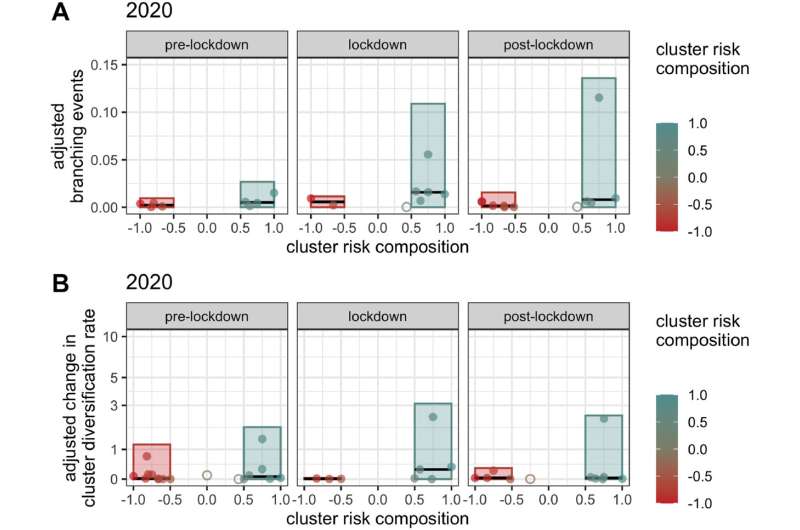
While the overall number of new HIV diagnoses in British Columbia (B.C.) continues a decades-long decline, epidemic monitoring during lockdown enabled rapid detection of a sharp increase in transmission within some groups (clusters) associated with PWUD.
"We're seeing the significant impact of converging public health threats within an extremely vulnerable population," says senior author Dr. Jeffrey Joy, an assistant professor in UBC's department of medicine and senior scientist at BC-CfE. "HIV transmission amongst people who use drugs had been relatively stable, but there was a sudden spike in select groups during lockdown."
In contrast, HIV clusters associated with MSM experienced a decline in transmission to a low-level rarely seen in the previous three years. The researchers say reduced social contacts and increased time at home are factors that likely contributed to reduced transmission in the MSM community.
"While lockdown measures reduced risk factors for some populations, other communities experienced pressures that greatly increased their risk," adds Dr. Joy.
Access to HIV care 'essential'
To explain the sudden growth of some clusters associated with PWUD, the researchers point to a reduction in access and engagement with HIV care and prevention services during the lockdown period. Their analyses revealed significantly lower rates of patients starting antiretroviral therapy (ART), pre-exposure prophylaxis (PrEP) prescription dispensations, viral load testing, HIV testing, and importantly, visits to overdose prevention services and safe consumption sites.
"These services are the frontline defense in the fight against HIV/AIDS. Many of them faced disruptions, closures, capacity limits and other challenges," says first author Rachel Miller, a research assistant at BC-CfE and recent graduate from UBC's Bioinformatics Graduate Program.
The researchers spoke with public health teams and healthcare providers who reported that some PWUD populations became more difficult to reach in the early days of the pandemic. A combination of factors, including housing instability and diminished trust, increased barriers for many individuals who normally receive HIV services.
As restrictions eased, engagement with HIV services rebounded but remained below pre-lockdown levels through the summer of 2020.
"Maintaining access and engagement with HIV services is absolutely essential to preventing regression in epidemic control and unnecessary harm," adds Miller. "We need to be increasingly attentive and consider innovative targeted solutions to ensure that measures we put in place to address one health crisis don't inadvertently exacerbate another."
Preventing long-term ripple effects
While the increase in HIV transmission was limited to a small number of clusters, the exponential nature of viral transmission means that even a limited period of variability can have serious downstream effects. After lockdown restrictions eased in B.C., some HIV clusters continued to experience elevated levels of growth for over a year.
"It is critical to detect and respond to even small changes in transmission because the downstream impacts can be significant and long lasting," says Dr. Joy. "As a global leader in HIV epidemic monitoring, BC-CfE is well-positioned to detect changes in near real-time so that we can respond rapidly and direct resources accordingly."
In 2020, B.C. marked a milestone when it surpassed the UNAIDS 90-90-90 target and recorded historically low levels of new HIV infections. The researchers say the new study highlights the need to remain vigilant.
"B.C.'s success remains strictly dependent on the programs and services we've put in place to support people at-risk and living with HIV/AIDS," says Dr. Julio Montaner, executive director and physician-in-chief at BC-CfE and UBC Killam Professor of Medicine. "This study reinforces that we can't take our foot off the gas, as the ripple effects can be devastating and risk undermining the progress we have made to date."
More information: Rachel L. Miller et al, Impact of SARS-CoV-2 lockdown on expansion of HIV transmission clusters among key populations: A retrospective phylogenetic analysis, The Lancet Regional Health—Americas (2022). DOI: 10.1016/j.lana.2022.100369





















