November 14, 2022 feature
Using CRISPR-interference and single-cell transcriptomics to systematically examine inflammatory reactive states
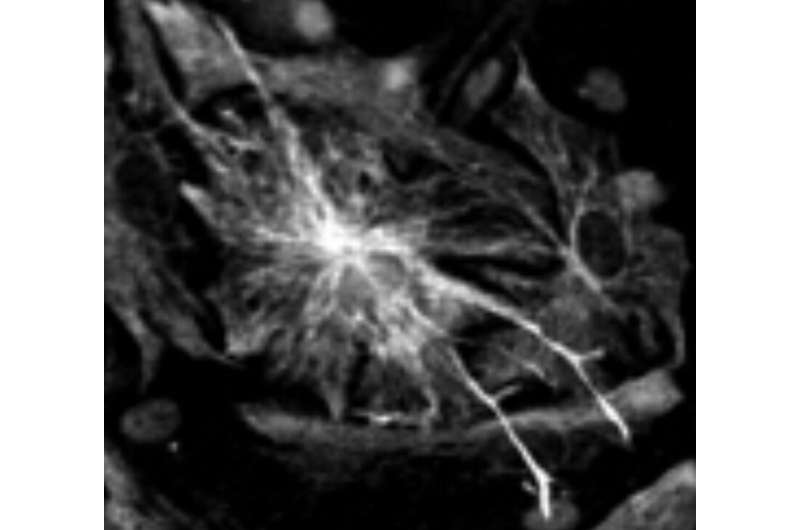
Astrocytes or astroglia, the largest glial cell population in the central nervous system (CNS), perform numerous vital functions. Among other things, these glial cells (i.e., cells supporting functions of the nervous system) are involved in regulating the flow of blood in the brain and repairing the brain or spinal cord after infections or traumatic injuries.
When the CNS is injured or inflamed, astrocytes become highly reactive, following unique cellular signatures that are specific to a context or neural event. While the reactive cellular signatures of astrocytes are now well-documented, the molecular mechanisms underlying them are still poorly understood.
Researchers at University of California, Vanderbilt University and Icahn School of Medicine at Mount Sinai have recently carried out a study aimed at better understanding the molecular underpinnings of the distinct astrocyte reaction patterns liked with different inflammatory states, using a combination of genetic techniques. Their findings, published in Nature Neuroscience, allowed them to identify different inflammatory reactive signatures that were regulated by a specific protein.
"My project was built around the idea of using CRISPR-based functional genomics (i.e., a genetic perturbation technique) to systematically study the cellular processes driving astrocyte reactivity, which can be broadly understood as how astrocytes respond to insults to the central nervous system," Kun Leng, the first author of the paper from the Kampmann lab at UCSF, told Medical Xpress. "Since reactive astrocytes are induced under a large variety of pathological contexts which can be hard to model in vitro, I chose to focus on astrocyte reactivity induced by inflammatory cytokines (i.e., signaling molecules that promote inflammation)."
The experimental methods used by Leng and his colleagues were inspired by a 2017 paper by Shane Liddelow published in Nature. In this work, Liddelow showed that that the cytokines IL-1α+TNF+C1q, which are released by activated microglia in vivo, induced a form of inflammatory reactivity in vitro that was pathological and may be involved in certain human neurodegenerative and neuroinflammatory diseases.
"Since a cell state is to a large extent determined by a cell's gene expression profile, a critical tool that enabled us to identify distinct inflammatory reactive states induced by IL-1α+TNF+C1q was single-cell RNA-sequencing, which captures the gene expression profile of individual cells," Leng explained. "This allowed us to identify markers of these states (i.e., expressed genes that were relatively distinct to either of the two inflammatory states we observed)."
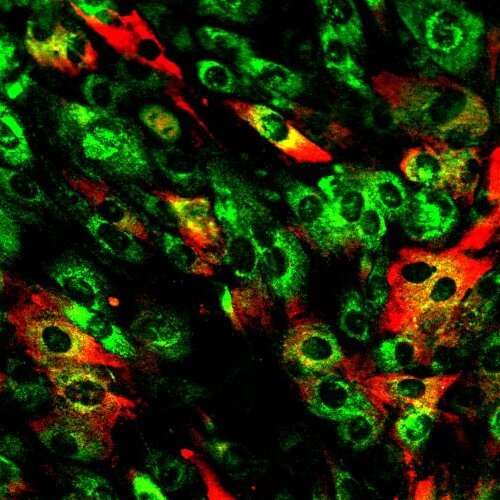
Leng and his colleagues observed two different inflammatory reactive states induced by the cytokines identified by Liddelow, and then identified genetic markers of these states. Subsequently, they conducted flow cytometry experiments, which also enable the close observation of individual cells. In these experiments, they used antibodies against these markers, to determine how perturbing certain gene transcription factors, kinases or receptors using genetic perturbation affected the balance of the two states.
"From a methodological perspective, our study was the first to apply CRISPRi screening, which requires a large number of cells (in the range of hundreds of millions), to iPSC-derived astrocytes," Leng said. "We were able to produce iPSC-derived astrocytes in a scalable fashion by building upon prior work identifying a suitable commercial astrocyte culture media as well as work which showed acceleration of astrocyte differentiation through overexpression of gliogenic transcription factors. Although there are limitations to studying astrocytes in vitro (as for any cell type), we believe that applying CRISPR-based screening to iPSC-derived astrocytes will nonetheless be useful for studying important aspects of astrocyte biology."
The recent work by this team of researchers provides new valuable insight about the genetic markers regulating different inflammatory reactive states in the CNS. Essentially, Leng and his colleagues showed that a mixture of cytokines can induce distinct cell states through mutually counter-regulatory signaling pathways.
Notably, the genetic markers influencing the signatures they identified were previously found to be upregulated in the brains of people affected by several neurological conditions, including Alzheimer's disease and hypoxic-ischemic encephalopathy (i.e., a brain injury that occurs as a result of decreased flow of oxygen to the brain). In the future, their work could inform the development of new therapeutic tools to selectively modulate specific aspects of inflammatory astrocyte reactivity, thus potentially improving the current understanding and treatment of some neurological conditions.
In their next studies, the researchers would like to investigate the functions of the two inflammatory reactive astrocyte states that they observed in their experiments. In addition, they plan to translate their strategies for regulating these reactivity states into tools that would allow medical researchers to selectively amplify or inhibit them.
"The next frontier for us is now to establish CRISPR screens for astrocytes and other cell types in living mice," Martin Kampmann, senior author of the paper, told Medical Xpress. "This will enable us to understand what controls cell states in the context of the brain in health and disease, and uncover how we can reprogram cell states for therapeutic benefit."
More information: Kun Leng et al, CRISPRi screens in human iPSC-derived astrocytes elucidate regulators of distinct inflammatory reactive states, Nature Neuroscience (2022). DOI: 10.1038/s41593-022-01180-9
© 2022 Science X Network



















