COVID vaccines also help protect HIV patients
People infected with HIV who receive antiretroviral therapy form antibodies against SARS-CoV-2 after being vaccinated against COVID with mRNA vaccines. Their immune response to the vaccination is, however, less strong than that of healthy people. A third vaccination reduces this gap.
These results emerged from a study with a total of 91 participants conducted by a research team led by Professor Ingo Schmitz, head of the Department of Molecular Immunology at Ruhr University Bochum, Germany. The researchers published their findings in the journal Frontiers in Immunology of 2 December 2022.
Vaccine protection in patients with acquired immunodeficiency
Studies have shown that the vaccines against SARS-CoV-2 protect otherwise healthy people quite well against severe COVID-19. Up to now, it has remained unclear whether this is also the case for people with acquired immunodeficiency.
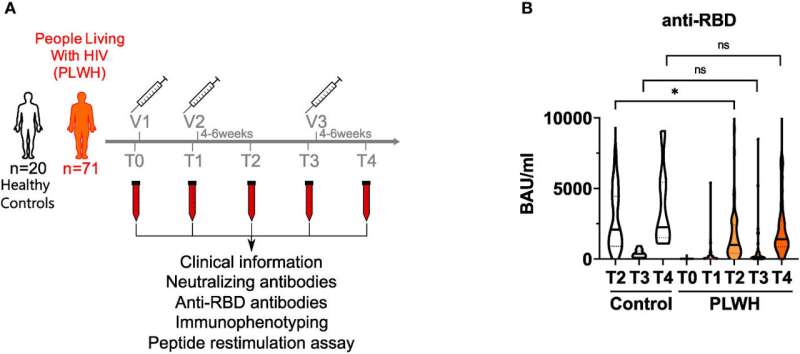
The research team headed by Ingo Schmitz and Dr. Anja Potthoff from the Walk in Ruhr (WIR) Zentrum für Sexuelle Gesundheit und Medizin (Center for Sexual Health and Medicine) at the university hospital of Ruhr University Bochum conducted a study with 71 HIV-positive participants who were receiving antiretroviral therapy. In addition, 20 HIV-negative control subjects took part in the study. After the first, second and third vaccination with the Biontech/Pfizer mRNA vaccine, they analyzed the immune response of each participant.
"We found that the vaccination leads to this group forming antibodies, too, but less well than is the case for healthy people," says Ingo Schmitz. "Seeing as this gap was reduced after a third shot, we believe that booster vaccinations should be recommended."
Surprisingly good cellular immune response
The researchers were surprised to discover that the cellular immune response mediated by T-helper cells was just as good in HIV-positive as in HIV-negative people.
"This is despite the fact that it is precisely these T-helper cells that are attacked by the HI virus and are reduced in number in HIV-positive people," says Ingo Schmitz. Since T-helper cells are longer lived than antibodies, this might indicate that HIV-positive people are protected by the vaccine more or less as long as HIV-negative people.
More information: Clara Bessen et al, Impact of SARS-CoV-2 vaccination on systemic immune responses in people living with HIV, Frontiers in Immunology (2022). DOI: 10.3389/fimmu.2022.1049070




















