April 18, 2023 report
This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
No link found between mRNA COVID-19 vaccination and retinal vascular occlusion
Researchers at Case Western Reserve University and the Cleveland Clinic in Cleveland, Ohio, have investigated the potential link between new-onset retinal vascular occlusion (RVO) after receiving the COVID-19 vaccination and compared the relationship with two historically used vaccinations.
With a sample size of more than 3 million patients, the findings published in JAMA Ophthalmology suggest that mRNA COVID-19 vaccination was not associated with newly diagnosed RVO.
The study, "Risk of New Retinal Vascular Occlusion After mRNA COVID-19 Vaccination Within Aggregated Electronic Health Record Data," was needed to follow up on recent literature describing new-onset RVO occurring acutely after messenger mRNA COVID-19 vaccination. Because RVO can cause vision loss or blindness, an epidemiologic investigation evaluating this potential association is of great importance to public health. An Invited Commentary by Lee M. Jampol and Maureen G. Maguire has been published in the same journal issue.
It is also important that the public be aware that many studies like this will be required to separate the noise of a global medical event from actual disease data. There will be correlations between the COVID-19 mass vaccinations and every form of ailment. The main driver in these correlations is the shared event of people getting vaccinated, almost everyone everywhere all at once.
For instance, the vaccine could be correlated to people around age 40 needing glasses for the first time. While needing glasses for the first time happens every year to this age group, only comparing this to a shared medical experience the cohort has in common (getting vaccinated) could make the events appear connected, even though they are not.
This was a big part of what previously caused people to fear childhood vaccinations, as symptoms of autism arise around the same time children get vaccinated. Add to that an increase in understanding and early diagnosis of autism along with active misinformation campaigns about the trace amounts of mercury used as a stabilizer, and people began to believe there was a connection when there was none.
When the medical community removed mercury from vaccines, autism diagnosis rates continued to climb, again because of recognition and diagnosis advances. The false conclusion based on correlative thinking would be that trace amounts of mercury stabilizer in the vaccines prevented some autism cases, which is why correlations alone are not science and correlations in studies are not considered causation. So a study that finds a null result, an absence of a link between a vaccine and any given disease, can be a tremendous public health service even if the only curative discovery is correct information.
To investigate how often patients are diagnosed with new RVO acutely after the mRNA COVID-19 vaccine, researchers compared current data with past vaccines for influenza, tetanus, diphtheria, and pertussis (Tdap).
The study used a retrospective population-based cohort design using the TriNetX Analytics platform, an electronic health record research network containing the deidentified data of more than 103 million patients. Data on patients within the 103 million were searched for vaccinations and instances of newly diagnosed RVO within 21 days of vaccination.
Out of 3,108,829 age-appropriate patients who received the mRNA COVID-19 vaccine, 104 (0.003%) patients had a new diagnosis of RVO within 21 days of vaccination. Compared to the rate at which people are statistically diagnosed with RVO yearly (~150 per 100,000 individuals), 0.003% is about a third of what would be expected in a 21-day span (~58 per 100,000 individuals per year).
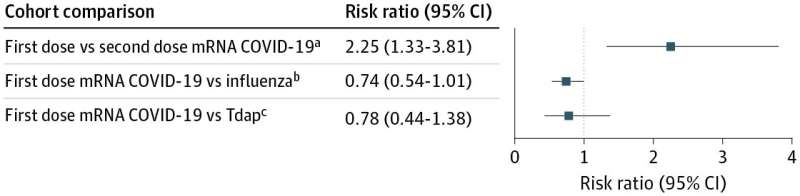
Diagnosis after the first dose of mRNA COVID-19 vaccination was not significantly different from that after influenza or Tdap vaccinations. However, it was more than twice the rate compared with the second dose of mRNA COVID-19 vaccination (~26 per 100,000 individuals per year). If this had been a study looking for a correlation between the mRNA COVID-19 vaccine and reductions in RVO diagnoses, an argument could have been made that it found one, which of course, it did not.
One possibility for the low numbers of RVO diagnoses could be that RVO symptoms can begin subtly, and visiting the eye doctor during a pandemic because of slightly fuzzy vision might not have been a priority.
Another possibility is that the agreed-upon rate at which RVO occurs is too high, and capturing data from millions of individuals around an arbitrary time point is revealing this.
Alternatively, it could be that rare diseases with low occurrence rates (0.15% yearly) do not fall neatly into arbitrary 21-day timeframes, which could imply a risk in conducting a study like this. Had a statistical clustering been reversed with RVO diagnosis rates 3 or 6 times greater than expected, the study could be seen to confirm an association when none existed.
The findings of this study suggest that RVO diagnosed acutely after COVID-19 vaccination occurs extremely rarely, and no evidence was found suggesting an association between the mRNA COVID-19 vaccination and newly diagnosed RVO.
While no further inquiry into RVO and mRNA COVID-19 vaccine connections appears warranted, the sheer volume of diseases awaiting similar correlative study will likely find a significant looking signal somewhere. When that happens, researchers, clinicians, science reporters and the general public should all repeat to themselves three times in a calm, authoritative voice, "Correlation does not imply causation, correlation does not imply causation, correlation does not imply causation."
More information: Ian Dorney et al, Risk of New Retinal Vascular Occlusion After mRNA COVID-19 Vaccination Within Aggregated Electronic Health Record Data, JAMA Ophthalmology (2023). DOI: 10.1001/jamaophthalmol.2023.0610
Lee M. Jampol et al, No Red Flags for Risk of Retinal Vascular Occlusion After mRNA COVID-19 Vaccination, JAMA Ophthalmology (2023). DOI: 10.1001/jamaophthalmol.2023.0925
© 2023 Science X Network




















