This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Psychiatrist discusses the complexities of ketamine treatment and the risks of at-home use
When administered correctly and under the supervision of a professional, ketamine can be a life-changing treatment for major depression. But following regulatory changes put in place during the COVID-19 pandemic that made telemedicine more accessible, the drug's off-label, unsupervised use has skyrocketed despite limited data supporting the safety and efficacy of that practice.
For the past 25 years, Gerard Sanacora, MD, Ph.D., George D. and Esther S. Gross Professor of Psychiatry, has been involved in all aspects of ketamine research from rodent models to clinical implementation. We spoke with Sanacora about the complexities of ketamine treatment and the risks of at-home use.
What is ketamine, and what is it used to treat?
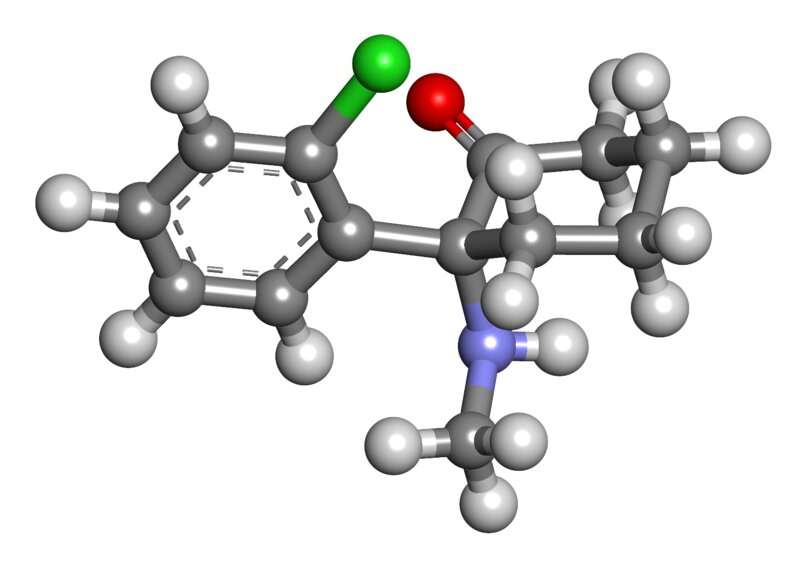
Ketamine is an FDA-approved treatment as an anesthetic drug. But when we talk about ketamine, it is important to note that it is what we call a racemic mixture. So, it has both S- and R-enantiomers, or molecules that are mirror images of each other. When we say "ketamine," we're usually talking about racemic ketamine.
S-ketamine is just the S-enantiomer, and this is the one that is thought to induce an anti-depressant response. The U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) have both approved S-ketamine given intranasally with a very rigorous risk evaluation mitigation strategy for the treatment of treatment-resistant depression and in the U.S. for depression associated with suicidal ideation.
The key point here is intranasal S-ketamine, under the brand name SPRAVATOÒ, can only be used under very controlled conditions. But we're in this very unique situation where nobody can stop people from using racemic ketamine, which contains S-ketamine, any way they want. This is because the FDA approved racemic ketamine 60 years ago as an anesthetic and didn't put any restrictions on it. So when the FDA introduced strict S-ketamine regulations to make sure it was being used safely and responsibility, there was this big loophole that people get around by simply not using S-ketamine. They just use the older racemic ketamine, which has no safety requirements associated with it.
How is S-ketamine administered, and how well does it work?
S-ketamine is regulated very tightly. It has to be delivered intranasally, in a certified health care setting under the supervision of a health care professional, and patients must remain in the facility for two hours after dosing. And there are very strict requirements about the pharmacies that can distribute it.
There is incredibly strong data suggesting the efficacy and overall safety of S-ketamine in the treatment of treatment-resistant depression and major depression associated with suicidal ideation. The further away you get from that, the less confident you can be in anything. That's my overall message. Once you start saying, "Well, I'm not going to use S-ketamine, I'm going to use racemic. And I'm not going to get it intranasally, I'm going to get an IV. And I'm going to change the dose and I'm going to use it in people with bipolar disorder." That's when we are less confident about what we know.
At the height of the pandemic, regulations loosened around telemedicine. How has this affected access to ketamine treatment?
For S-ketamine, not all that much. They did have a small loophole that patients could be treated at home if there was a health care provider that could go to their house.
But, it allowed people to do telemedicine visits and just use racemic ketamine because there's no regulation of it. Now we're hearing stories of people calling and talking to some health care professional, and within five minutes, they're being sent the drug to do at home without supervision. But is that safe or effective? We have no real data to support that.
What have been the consequences of the expansion of ketamine access?
There are real risks associated with any version of ketamine. It is an anesthetic. If you get enough of it, you will become completely sedated—that's always a risk associated with it. But it has other physiologic effects on heart rate and blood pressure that can be pronounced. For most people, this is not a major issue. But if you are somebody that has an elevated risk of a cardiovascular event, there can be very serious consequences. For instance, if somebody has significant coronary artery disease or has an aneurysm, ketamine could kill them on the spot.
There are also psychological risks. When you take either form of ketamine, it has significant effects on cognition, meaning that you're no longer thinking clearly at all. There are large amounts of data suggesting that your ability to make rational, correct decisions is completely disrupted when you take ketamine as long as it's in your system. Usually, this is about an hour and a half to two hours. It can also dramatically alter perceptions. People can hear things differently, see things differently, feel things differently—this can be really scary to some people and cause them to act differently than they would without the drug in their system. The physiological and psychological reasons are the main reason the FDA declared the drug safe only in a health care facility under supervision.
There are two other risks that are a little bit more complicated. One is related to the real care of people with serious mental illness. Ketamine is not a miracle cure. This is not a treatment to be given in isolation. All of the studies presented for consideration of FDA-approval were done with very close psychiatric follow up. It is incredibly naïve and uninformed to think ketamine alone will make your depression go away. It's a part of a treatment plan, not the treatment plan. It should be given as part of an overall treatment plan with a mental health professional. In fact, the FDA approval for ketamine also states that it has to be used along with an oral anti-depressant. It's not even approved to be used alone. These ketamine clinics that provide the treatment without close follow-up of some type being provided by a mental health professional, in my mind, are a very dangerous thing, because they aren't providing the comprehensive mental health care that these patients need.
Finally, there is a risk to society and the drug reaching black markets. Ketamine is a known drug of abuse. In fact, some places—including parts of Asia and the U.K.—it became a major drug of abuse. Especially right on the heels of the opioid epidemic, there's this real concern that we have this flood of ketamine reaching the black market, where it's going to follow into recreational use leading to misuse. This is why when the FDA approved S-ketamine, it put very strict regulations on how pharmacies can distribute it. But I guess they didn't foresee that people would use racemic ketamine instead.
In your opinion, what policies should be put in place, if any, to improve safety for patients?
I think the best approach is always to gather more data to better understand what the actual risks and benefits are to both individuals and society. I don't necessarily think we should stop the use of off-label ketamine, but it should be studied more rigorously. The best way to do that is through some type of registry, which I've been trying to form for years. But how you form one is tricky, and there's a lot of concern that if you make this registry too restrictive, you would reduce accessibility to patients. There's always that fine balance—you don't want to restrict access to patients who are trying to get care, but on the other hand, you want to make sure that you're using a drug that is safe and effective and that you have a way of collecting data.
Are ketamine clinics a good place to seek treatment?
This idea of having ketamine clinics that stand alone are something that we must think really carefully about. This is because they're not seeing patients and deciding what the best treatment is—they only have one treatment. They don't provide comprehensive care. As I said before, this is not a treatment in and of itself. It's part of the whole treatment plan. Let's say somebody has diabetes and I have an insulin clinic. I'm going to give you insulin, but I'm not going to take care of any other part of your diabetes. We're not going to talk about diet or lifestyle changes. We're not going to talk about anything else. I'm just going to give you the insulin. That's the real danger with ketamine clinics. If a patient has a crisis at two in the morning, they don't have a way to contact a mental health professional. This is my biggest concern about ketamine treatment: It is critical for it to be a part of a comprehensive mental health plan, not in isolation.
Is there anything else you want to add?
I would like to highlight what interventional psychiatry at Yale is like. What we are trying to do is provide this treatment in a way that provides the greatest accessibility to people, but also in a way that's highly responsible. This involves us working closely with community providers and referring mental health care professionals to ensure patients are receiving close follow-up and more comprehensive treatment services. We perform thorough prior evaluations for all patients referred for treatment and make decisions based on the patients' individual situations as to the best treatment approach. This could be treatment with ketamine, esketamine, one of the other treatments we offer within our interventional services, or as we very commonly recommend, other forms of treatment outside of our service for patients for whom we believe an alternative treatment would be most appropriate at this point in their care. Furthermore, we make great efforts to collect data that can help us learn from our experience and ultimately develop and provide a more effective and efficient treatment model.
The most important thing I'd like readers to take away is ketamine treatment needs to be integrated into a comprehensive mental health care plan. This is not a standalone.



















