This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Study reveals high prevalence of alcohol, opioid use among patients with Crohn's disease
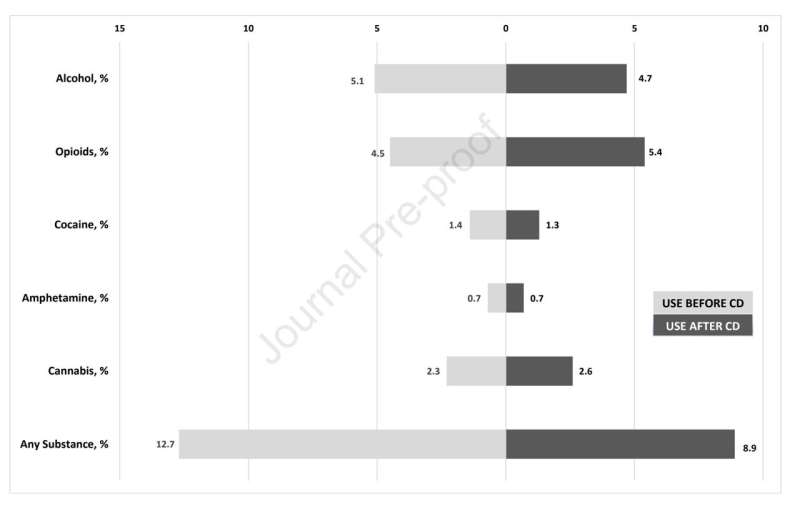
Newly diagnosed people with Crohn's disease (CD) in the United States are more likely to experience drug and alcohol use compared with the general population, according to a recent study led by Johns Hopkins Medicine researchers. The study, which used data from Medicaid between 2010 and 2019, found that 16.3% of enrollees had some form of substance use at the time of being diagnosed with CD, with alcohol and opioids being the most commonly used substances.
According to the Crohn's and Colitis Foundation, more than 500,000 people in the U.S. have Crohn's disease, a chronic inflammatory bowel disease (IBD) that affects the lining of the digestive tract. It causes abdominal pain, diarrhea, weight loss, anemia and fatigue. Experts say alcohol and opioid use can worsen these symptoms.
"About a quarter of these patients experience depressive symptoms, which have well-established connections with substance use disorders," says Victor Chen, M.D., assistant professor of medicine at the Johns Hopkins University School of Medicine and lead author of the study. "Alcohol and opioid use and Crohn's disease symptoms are likely a chicken-and-egg situation—more substance use can worsen Crohn's symptoms, but more severe symptoms can increase substance use to mask the discomfort."
Chen says there is limited data on substance use among patients newly diagnosed with Crohn's disease, which was one of the driving factors behind the study, published in the journal Gastro Hep Advances.
The researchers analyzed data from 37,323 Medicaid enrollees, and results revealed that 16.3% of patients newly diagnosed with Crohn's disease reported some form of substance use. Alcohol and opioids were the two most commonly used substances (8% respectively), followed by cannabis (4.3%), cocaine (2.3%) and amphetamine (1.3%). Tobacco use was not included in the study.
Per the 2019 National Survey on Drug Use and Health (NSDUH), 5.8% of the general population over the age of 12 reported heavy alcohol use, defined as five or more drinks for men and four or more drinks for women during the same session on at least five of the past 30 days. NSDUH also reported that 3.7% of the U.S. population over age 12 stated opioid misuse in the previous year.
Chen says one limitation of the study is the different data collection methods between NSDUH (self-reported surveys) and Medicaid (clinician-documented billing codes), which may account for part of the findings.
Still, he adds, the results suggest that physicians need to be more aware of substance use among patients with Crohn's disease, given some substances' potential to worsen disease symptoms.
"Alcohol or substance use screening is the first step," Chen says. "Then, for patients with unhealthy substance use, I would encourage at least referrals to addiction [specialists] or begin some of the addiction treatments in the GI clinic if the gastroenterologist is familiar with them."
More information: Po-Hung Chen et al, Substance use among patients with incident Crohn's disease in the United States, 2010 to 2019: a Medicaid observational study, Gastro Hep Advances (2023). DOI: 10.1016/j.gastha.2023.03.019



















