This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Model blood-brain barrier could improve newborn meningitis treatment
Investigators in Israel and Italy have developed a model of the blood-brain barrier, studies of which may lead to prevention of meningitis in newborns. The research is published in Microbiology Spectrum.
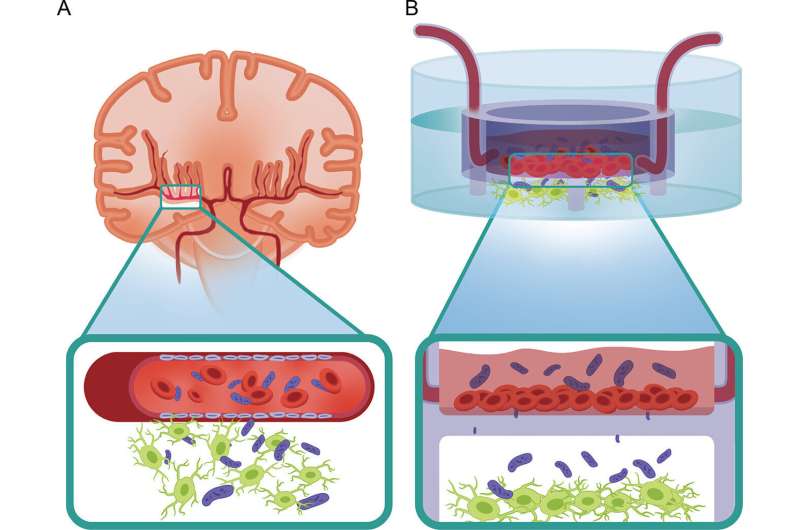
The investigators further developed a platform called organs-on-a-chip—invented during the 2000s—to construct the model. These devices, which are modeled after microchips, contain tiny channels lined with living human organ cells and others with human blood vessel cells. In this case, the researchers grew human neuronal and glial cells within the chip, atop cells from human vasculature, the latter separated from the other cell types by a membrane, as they are in humans and other animals.
The investigators then tested the chips by infecting each with one of several meningitis causing strains of E. coli that infect newborns. They had isolated these strains from cases of newborn meningitis, an infection that cannot be prevented by the standard vaccination against meningitis. The meningitis strains caused the neurons growing in the chips to degenerate, and ultimately, to die.
The overarching goal of developing the organ-on-a-chip was to hasten drug development for the treatment of newborn meningitis, said corresponding author Ben M. Maoz, Ph.D., Department of Biomedical Engineering, Sagol School of Neuroscience, and Sagol Center for Regenerative Medicine, Tel Aviv University, Tel Aviv, Israel.
Newborn meningitis infects around 1% of all newborns, with a mortality rate of about 50% in developing countries, and 8-12.5% in industrialized countries. "Those who recover are prone to developing neurodegenerative disease," Maoz said.
However, between 60 and 90% of experimental drugs that work when tested for safety and efficacy in animals fail when tested in humans, which is not surprising since animal models are rough approximations of human physiology, at best. Testing drugs on organs-on-a-chip will be far more accurate at predicting efficacy and safety in humans, said Maoz. It will also be much quicker and less expensive than testing in animals, providing answers in hours rather than weeks, months or even years.
The organ-on-a-chip can also be used to determine how other pathologies affect the blood-brain barrier, said Maoz. Maoz and his collaborators currently are investigating how Parkinson's disease and certain drugs such as methamphetamine affect the chip to determine how they might affect the blood-brain barrier.
They have found that crystal meth causes neurotoxicity by opening the blood-brain barrier, allowing toxic materials from blood to enter the brain, said Maoz. In the case of Parkinson's disease, "we see vascular dysfunction which causes higher permeability."
More information: Rossana Rauti et al, Insight on Bacterial Newborn Meningitis Using a Neurovascular-Unit-on-a-Chip, Microbiology Spectrum (2023). DOI: 10.1128/spectrum.01233-23


















