This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Partial liver transplants for kids could be key to preventing waitlist deaths and improving outcomes
Dozens of children die each year in the U.S. while waiting for a new liver. A new analysis led by University of Pittsburgh and UPMC physician-researchers suggests that greater use of partial liver transplants—either from a living donor or by splitting a deceased donor's liver for two recipients—could save many of these young lives.
Published in the July issue of Liver Transplantation, the study found that transplant centers offering partial liver transplants, also known as technical variant grafts (TVGs), had fewer waitlist deaths than those providing traditional whole deceased donor liver transplants only. The findings suggest that more training, support and collaboration across centers to support TVG transplants could help eliminate pediatric liver waitlist mortality.
"Since the first successful liver transplant in Pittsburgh 42 years ago, we've made tremendous advances, but significant gaps still remain nationally," said lead author George Mazariegos, M.D., chief of pediatric transplantation at UPMC Children's Hospital of Pittsburgh and Jamie Lee Curtis professor of surgery and critical care medicine at Pitt's School of Medicine. "It's tragic that 6% of children are still dying on the liver transplant waitlist in the United States. The goal is zero."
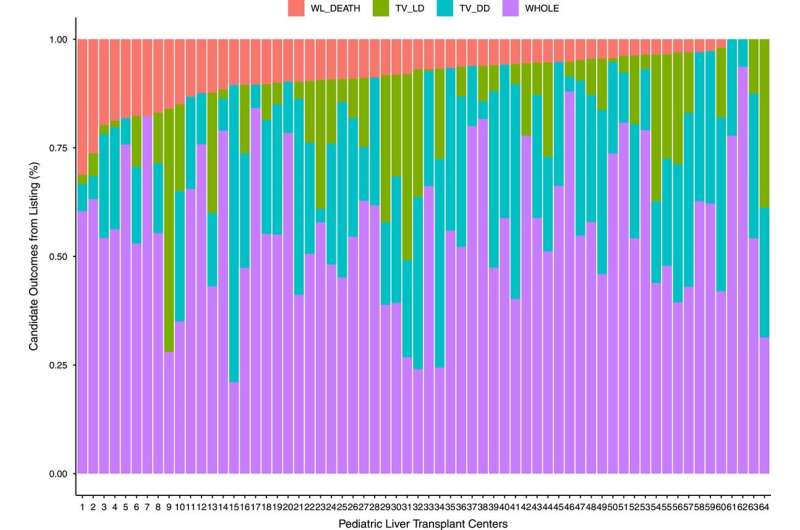
Mazariegos and his multi-center collaborators analyzed U.S. pediatric liver transplant data from the national Organ Procurement and Transplantation Network. From 2004 to 2020, across 64 transplant centers that performed at least 10 pediatric liver transplants during that time period, 7,842 children received liver transplants, and 657 children died on the waitlist. At individual centers, waitlist mortality rates varied from 0% to 31%.
"The first takehome message from this study is that we need urgency on a national level to address waitlist mortality," said Mazariegos, who is also director of pediatric transplantation at the Hillman Center for Pediatric Transplantation and a member of the McGowan Institute for Regenerative Medicine. "This is a solvable problem, and we can fix it today if we work together to identify critical challenges and best practices."
Next, the researchers evaluated use of TVGs from living or deceased donors. At individual centers, the proportion of total transplants made up by TVGs ranged from 0% to 76%. Higher use of TVGs was linked with lower waitlist mortality and improved outcomes. In contrast, organ availability did not influence waitlist mortality.
"The second take-home message from the study is that center practices drive patient outcomes, not the vagaries of organ availability," said Mazariegos. "It's up to each center to change what they're doing, refer patients to centers that have better outcomes or work collaboratively to achieve the best outcomes for their patients."
Comparing survival outcomes of patients with different types of grafts, the researchers found that recipients of living donor transplants had improved survival compared with either type of deceased donor graft. Survival was statistically similar between patients who received deceased donor partial or whole livers, which is notable because splitting a graft can potentially save two patients' lives instead of one.
"We need more training and support to develop technical variant graft programs and expertise at transplant centers across the country," said Mazariegos. "At the end of the day, it's about every center committing to giving every child the best opportunity to receive and thrive after their transplant. I strongly believe that the way forward is collaboration, not competition."
Mazariegos and his team previously launched the Starzl Network for Excellence in Pediatric Transplantation, a collaborative learning health system of 16 leading pediatric liver transplant centers in the U.S. and Canada that seeks to identify challenges and develop and share best practices in transplantation, including a focus on elimination of waitlist mortality in children awaiting transplant.
More information: George V. Mazariegos et al, Center use of technical variant grafts varies widely and impacts pediatric liver transplant waitlist and recipient outcomes in the United States, Liver Transplantation (2023). DOI: 10.1097/LVT.0000000000000091



















