This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Weight-loss treatment for kids in pediatric primary care shown to work best when it's family-focused
Obesity runs in families. That fact is at the root of an intensive, behavioral, family-based treatment developed by University at Buffalo researchers and targeted to children who are obese or overweight and their parents.
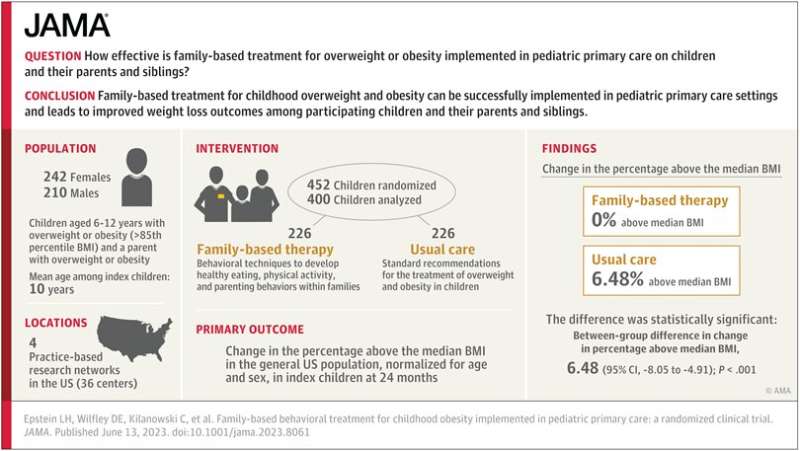
Previously available only in specialty clinics, this evidence-based treatment has now, for the first time, been implemented in a multicenter study carried out in four U.S. cities in children ages 6–12 in the primary care setting, where the vast majority of children receive care.
The study, published online June 13 in the Journal of the American Medical Association (JAMA), demonstrates that family-based treatment for obesity conducted in the pediatrician's office leads to improved weight-loss outcomes for the treated child and parent, and even extends to untreated siblings.
"This research shows that the healthy behaviors the treatment promotes extend beyond the parent and child being treated to potentially make the whole family healthier," says David C. Goff Jr., MD, Ph.D., director, Division of Cardiovascular Sciences, NHLBI. "What's more, the fact that this weight-loss study was implemented during the COVID-19 pandemic, when many adults and children gained weight, is noteworthy."
The study found that three times as many children in the treatment group (27%) as in the usual care group (9%) had a clinically meaningful reduction in median over body mass index (BMI) associated with improved cardiometabolic outcomes, such as blood pressure, lipids and glucose regulation.
Family focus is key
"Our study is the first to test family-based treatment in primary care for children 6–12 years old and it worked for the child, for parents and even for their untreated siblings," says Leonard H. Epstein, Ph.D., senior author, SUNY Distinguished Professor and chief of the Division of Behavioral Medicine in the Department of Pediatrics in the Jacobs School of Medicine and Biomedical Sciences at UB.
Epstein is internationally known for pioneering this behavioral, evidence-based, family-focused approach to childhood obesity.
"The success of this novel and powerful family-based treatment of childhood obesity, which Dr. Epstein and his colleagues have developed, helps ensure the health of these children," says Allison Brashear, MD, vice president for health sciences and dean of the Jacobs School. "It will not only impact them today but going forward as they adopt healthy practices for the rest of their lives."
The current work builds on more than 40 years of work by Epstein and colleagues, including a previous study in the primary care setting led by Teresa Quattrin, MD, UB Distinguished Professor in the Department of Pediatrics and senior associate dean for research integration in the Jacobs School.
Quattrin, also co-author on the JAMA paper, had successfully adapted this treatment for preschool children and parents with obesity in the primary care setting, demonstrating that outcomes for preschool-aged children who are overweight improve when both parent and child are treated compared to when only the child is treated.
Multiple people benefit
"Many families with obesity have multiple children with obesity, as well as parents with obesity," says Epstein, "but traditional treatment for childhood obesity only focuses on the child; it may provide ideas about healthier foods and the recommendation to be more active, but the parent is never an active target for intervention, nor is the parent taught positive parenting."
The usual treatment also doesn't focus on changing behaviors and is not administered by professionals with experience in behavior therapy.
By contrast, the family-based treatment in the JAMA study included eating and activity plans, education in parenting and behavioral techniques, and facilitation of support for positive behavior changes in both family and peer environments. Parent and child were seen together in individualized sessions that included reviews of self-monitored eating and activity levels, review of treatment manuals and handouts, and discussions about goal-setting for weight and behaviors.
Families met weekly for the first four months to learn the program, then bi-weekly and then monthly. Most treatment providers had experience working with families and also had master's degrees in either psychology, counseling, social work or dietetics.
The randomized clinical trial enrolled 452 children aged 6 to 12 years with one parent in primary care practices in Buffalo and Rochester, New York; Columbus, Ohio; and St. Louis, Missouri. Half of the children were randomly assigned to family-based treatment and half received the usual care; 27.2% of the children were Black, 8.8% were Latinx and 57.1% were white.
Children enrolled in the family-based treatment had a difference in percent over median BMI versus those receiving the usual care of 6.48%, while their parents had a reduction of 3.97% and their untreated siblings who were overweight had a reduction of 5.38%. The changes in percent over median BMI among family members were related, suggesting that the treatment results in modeling healthy behaviors and in real change in the shared family environment.
"Family-based therapy is unique in using up-to-date behavioral treatments to teach parents and children methods to eat healthier and be more physically active, and in the process teach positive parenting," says Epstein.
Primary care 'coaches'
The success of the behavioral interventions in the current study underscore what the authors perceive as a growing need for behavioral treatments in pediatric primary care in general.
"The results of the study underscore the need for 'coaches' in the primary care setting who can help with obesity treatment as well as many other behavioral problems, such as anxiety, depression, eating disorders and a host of other issues which require psychological support and behavior modification," says Quattrin, also a pediatric endocrinologist with UBMD Pediatrics.
More information: Leonard H. Epstein et al, Family-Based Behavioral Treatment for Childhood Obesity Implemented in Pediatric Primary Care, JAMA (2023). DOI: 10.1001/jama.2023.8061




















