This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Researchers link blood flow regulation in the brain and prognosis following cardiac arrest
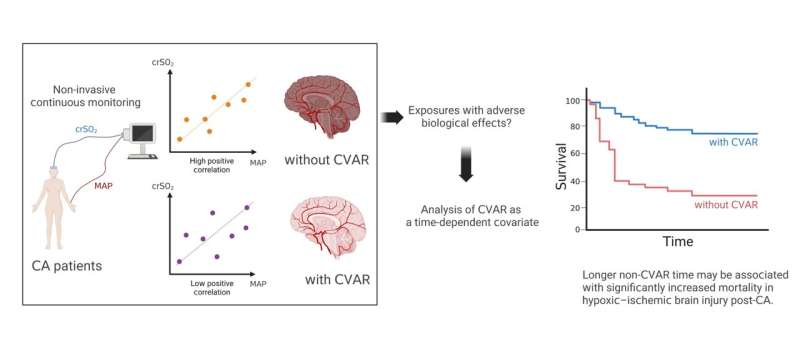
A group of researchers at Osaka University have used a noninvasive method to evaluate cerebrovascular autoregulation (CVAR) in patients following out-of-hospital cardiac arrest. The mortality rate increased significantly with the duration of time that CVAR was undetectable. The article, "Association between time-dependent changes in cerebrovascular autoregulation after cardiac arrest and outcomes: a prospective cohort study," was published in Journal of Cerebral Blood Flow and Metabolism.
It has been suggested that CVAR, a function that is present in the normal state, may be impaired after cardiac resuscitation. However, the relationship between CVAR function and patient prognosis has been unclear.
The research examined CVAR over time, using the moving Pearson correlation coefficient calculated from regional cerebral oxygen saturation and mean blood pressure data. The researchers performed a survival analysis using the presence or absence of CVAR as a time-dependent covariate.
The findings of this study may be useful in predicting neuroprognosis after cardiac resumption and may also help avoid early withdrawal of treatment in those who recover. In addition, they suggest that treatment and management that maintains proper CVAR after cardiac resumption may improve patient prognosis. This may then be applied to the management of post-cardiac arrest resuscitation, based on cerebral circulation, to optimize treatment for each individual patient.
Although standardization of treatment for out-of-hospital cardiopulmonary arrest has progressed and efforts to improve outcomes are being made worldwide, many patients still suffer neurological sequelae (hypoxic-ischemic brain injury, HIBI) even after return of spontaneous circulation.
It is known that if brain function is maintained normally, there is a mechanism (CVAR) that tries to maintain cerebral blood flow at a constant level even if systemic blood pressure changes, but until now, it was unclear whether such a reaction occurs in the brain after resuscitation. Cerebral regional oxygen saturation (crSO2), a measure of oxygen supply and demand balance in the brain, is affected by blood pressure, and the researchers focused on a method to evaluate the presence or absence of CVAR using this correlation.
The team used this correlation to evaluate the presence or absence of CVAR in the post-resuscitated brain and assessed its relationship to life expectancy.
In this study, the research group analyzed 100 patients with out-of-hospital cardiac arrest who were transported to the trauma and acute critical care center of the Osaka University Graduate School of Medicine.
CVAR was determined by calculating the moving Pearson correlation coefficient and by continuously monitoring crSO2 and mean blood pressure for 96 hours after return of spontaneous circulation. Assuming undetected CVAR time as a bad exposure for the organism (time-dependent covariate), the association with life prognosis was evaluated by Cox proportional hazards model.
CVAR was detected in all 24 patients with good neuroprognosis (Cerebral Performance Scale: CPC 1–2) out of 100 analyzed subjects and in 65 (88%) of 76 patients with poor neuroprognosis (CPC 3–5). The analysis using the Cox proportional hazards model showed that the survival rate decreased significantly as the undetected time of CVAR increased.
The results of this study have two major implications. First, the ability to identify subgroups with high mortality from early post-resuscitation clinical data can help identify populations that should receive enhanced therapeutic intervention. In addition, it may help to avoid early withdrawal of treatment from those who may recover. Secondly, the researchers believe that intensive therapeutic management that maintains proper cerebral perfusion suggests improved life outcomes, and that developing a systemic management approach based on cerebral perfusion may be a breakthrough in reducing post-resuscitation neurological sequelae.
More information: Jotaro Tachino et al, Association between time-dependent changes in cerebrovascular autoregulation after cardiac arrest and outcomes: A prospective cohort study, Journal of Cerebral Blood Flow & Metabolism (2023). DOI: 10.1177/0271678X231185658




















