This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers use machine learning to identify high-risk surgery patients
Researchers and physicians at the University of Pittsburgh and UPMC used machine learning to create and deploy an accurate and flexible model for predicting patients at high-risk for complications after surgery, according to a study published in JAMA Network Open.
Before the COVID-19 pandemic, the third leading cause of death globally was complications 30 days after surgery, killing about 4.2 million people each year. Identifying patients who are at high-risk for complications before they undergo surgery is critical to saving lives and lowering health care costs.
"Improving overall health of patients prior to surgery through prehabilitation can go a long way in improving outcomes for high-risk patients," said Aman Mahajan, M.D., Ph.D., M.B.A., chair of Anesthesiology and Perioperative Medicine, Pitt School of Medicine, and director of UPMC Perioperative and Surgical Services.
"However, identifying high-risk patients can be challenging for busy clinicians, who have to integrate the wealth of health data available and frequently perform additional testing and clinical assessments. We wanted to build an easy-to-use model that provides the health care team with an automated and accurate risk assessment quickly using existing data in the electronic health record."
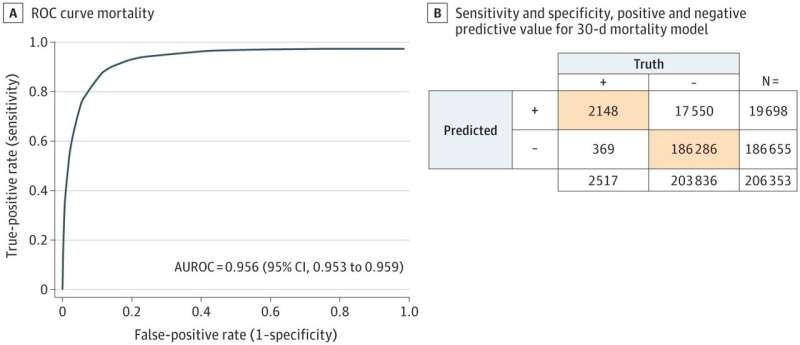
To create the model, Mahajan and Oscar Marroquin, M.D., chief health care data and analytics officer at UPMC, and their teams trained the algorithm to learn from the medical records of over 1.25 million surgical patients. The model focused on mortality and whether patients had a major cerebral or cardiac event, like a stroke or heart attack, after surgery. The model was then validated against another 200,000 patients who underwent surgery at UPMC.
After validation, the model was deployed across 20 UPMC hospitals. Every morning, the program reads the electronic medical record for patients who are scheduled for surgery and flags those determined to be high-risk. This notification allows clinical teams to better coordinate care and institute some prehabilitation in advance of their surgery, like making healthier decisions or even a referral to the UPMC Center for Perioperative Care, lowering their risk of complications. Clinicians can also run the model at any time on demand.
To gain a better understanding of how their model compared to the industry standard, Mahajan and his team compared it against the American College of Surgeon's National Surgical Quality Improvement Program (ACS NSQIP). While the ACS NSQIP is used at hospitals throughout the country, it requires clinicians to manually input patient information and cannot make a prediction if information is missing. Mahajan and his team found their model did a better job at identifying high-risk patients than the ACS NSQIP.
"We designed our model with the health care worker in mind," Marroquin said. "Since our model is completely automated and can make educated predictions even if some data are missing, it adds almost no additional burden to clinicians while providing them a reliable and useful tool."
As the model continues to be refined and developed, Mahajan and his team aim to train the program to predict the likelihood for sepsis, respiratory issues and other complications that often keep patients in the hospital after surgery.
More information: Aman Mahajan et al, Development and Validation of a Machine Learning Model to Identify Patients Before Surgery at High Risk for Postoperative Adverse Events, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.22285





















