This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Photon-counting CT can evaluate lung function
New CT technology allows for a comprehensive, simultaneous evaluation of lung structure and function, something not possible with standard CT, according to a study published in Radiology, a journal of the Radiological Society of North America (RSNA).
Chest CT is the imaging method of choice for analyzing lung disease and tracking changes over time. However, CT studies of lung function and perfusion, or blood flow, require dedicated protocols that cannot be combined.
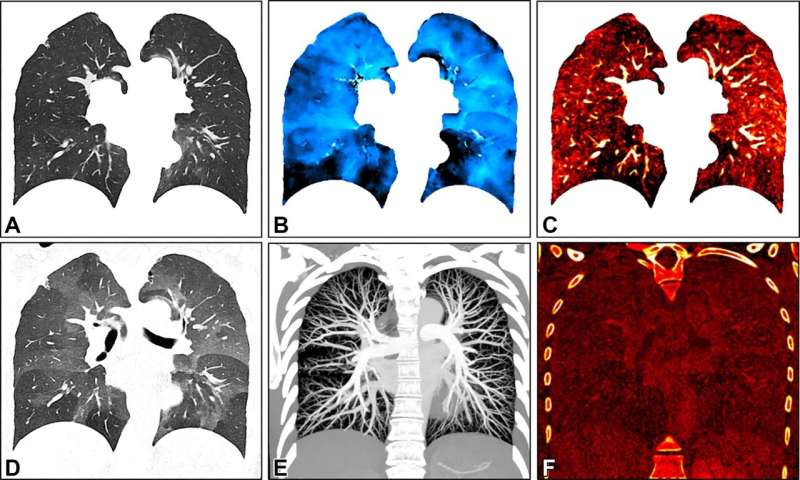
Researchers in Germany and the Netherlands developed a chest imaging protocol that yields information on structure and function of the lungs as a one-stop-shop procedure. The protocol uses recently introduced photon-counting CT technology. Photon-counting CT enables high image quality at a radiation dose below that of a standard chest CT. In addition, it provides better spatial resolution and options for spectral imaging, which uses energy information from the X-rays to characterize tissue composition. The new protocol requires advanced software but no additional hardware.
The researchers studied the protocol in 197 patients with clinically indicated CT for various known and unknown lung function impairment. After administration of an intravenous contrast agent, the photon-counting CT scan was taken when the patients inhaled. This was followed by a scan when the patients exhaled.
In 166 patients, the researchers were able to acquire all CT-derived parameters, for a success rate of 85%.
The protocol allowed for simultaneous evaluation of lung structure, ventilation, vasculature and perfusion of the parenchyma, the region of the lungs that contain the gas-exchanging alveoli. The alveoli are tiny air sacs where the lungs and the blood exchange oxygen and carbon dioxide during the process of breathing in and out. The protocol showed advantages over standard CT.
"The improvement in the contrast-to-noise ratio and spatial resolution of the pulmonary blood volume images was substantial," said study senior author Hoen-oh Shin, M.D., professor of radiology at the Institute of Diagnostic and Interventional Radiology at Hannover Medical School in Hannover, Germany. "In my opinion, the most important advantage is the significantly improved spectral resolution, which enables new applications such as functional imaging of the lungs with CT."
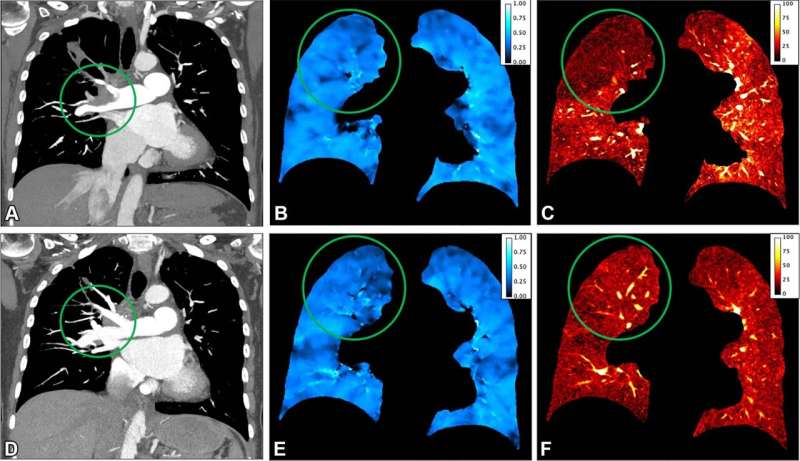
The photon-counting CT protocol has other promising applications in lung imaging. It can provide important preoperative identification of areas of emphysema and perfusion defects in patients with chronic thromboembolic pulmonary hypertension, a progressive disease caused by blood clots that do not clear from the lungs.
Postoperatively, the protocol allowed evaluation of surgical success and was helpful in assessing the lungs after lung or stem cell transplant procedures. It may also be useful in follow-up of chronic obstructive pulmonary disease and looking at pathological findings in the lung tissue.
"We believe that the proposed protocol is generally valuable for diseases with known or unknown lung function impairment," Dr. Shin said.
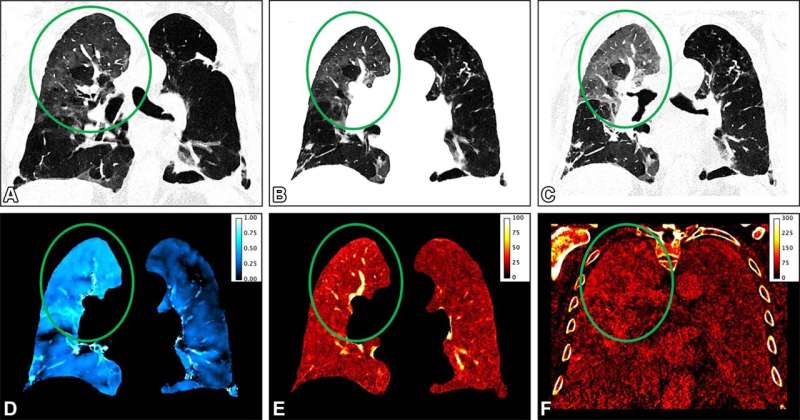
Dr. Shin and colleagues first applied the protocol to patients with interstitial lung disease, a group of diseases that cause progressive scarring of the lung tissue. They then expanded the applications to include post-COVID-19 condition where interstitial lung disease sometimes develops.
"With the proposed protocol, we have also been able to answer many other questions related to post-COVID-19 condition, such as the detection of acute and chronic pulmonary emboli on CT angiography, and we are currently investigating whether perfusion changes can be quantified in microvascular damage or inflammatory areas," Dr. Shin said.
The researchers are working to improve processing time and increase the robustness of the technique.
"Regional ventilation and perfusion depend on patient position and gravity, among other factors," Dr. Shin said. "Further studies are needed to assess the dependence on position and depth of breathing, as well as the reproducibility of the measurements."
More information: Sarah C. Scharm et al, Regional Pulmonary Morphology and Function: Photon-counting CT Assessment, Radiology (2023). DOI: 10.1148/radiol.230318





















