This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Optimizing tobacco cessation treatment with lung cancer screening
Lung cancer is the deadliest cancer in the United States, and 80% of lung cancer deaths are linked to one risk factor: smoking. While lung cancer screenings are a critical part of prevention and treatment for the disease and 15 million Americans qualify for yearly screenings, over half those eligible for screenings are still actively smoking. Without standard smoking cessation measures in place, the benefits of the screenings have not been fully realized.
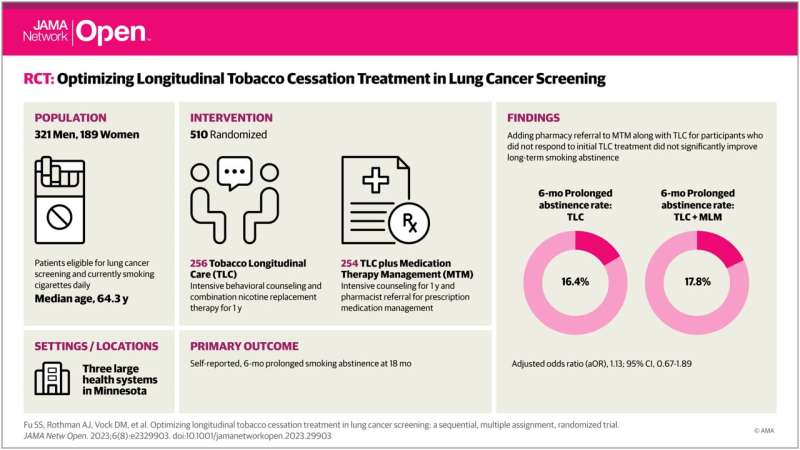
New research published in JAMA Network Open, led by the University of Minnesota Medical School, examined how different combinations of behavioral treatment and medication affect tobacco cessation and, going forward, how they can be used to increase the benefits of lung cancer screenings. Researchers from the School of Public Health, College of Liberal Arts, U.S. Department of Veterans Affairs and Allina Health also contributed to the study.
The Program for Lung Cancer Screening and Tobacco Cessation (PLUTO) trial tested different adaptive interventions based on the evidence-based Tobacco Longitudinal Care (TLC) program, in part to learn how best to incorporate TLC into annual lung cancer screening as a smoking cessation standard. The trial assessed the effect of adding a referral to prescription medication therapy management to the TLC program among participants who did not respond to initial TLC treatment—i.e. did not stop smoking—as well as the effect of decreasing the intensity of TLC among participants who did respond to initial treatment.
The study found:
- After initial TLC treatment, 80% of participants had not responded to treatment (were continuing to smoke cigarettes) and 20% had responded to treatment (early success with quitting).
- After 18 months of follow-up, the quit rate across the TLC intervention groups was 24%.
- Among participants who did not respond to initial TLC treatment, the quit rate for participants who additionally received a referral for medication therapy management was similar to the participants who received TLC without medication therapy management.
- Among participants who did respond to initial TLC treatment, the quit rate for those receiving TLC quarterly was 44% compared to 59% for those receiving TLC monthly.
The findings suggest that TLC was most effective when implemented without modification and does not need additional pharmacist resources. Integrating the TLC program—which consists of frequent telephone coaching and over-the-counter combination nicotine replacement therapy (NRT)—with lung cancer screening was feasible and associated with clinically meaningful quit rates.
"If we do not help people quit smoking, we will not adequately reap the benefits of lung cancer screening," said Steven Fu, a professor at the U of M Medical School, member of the Masonic Cancer Center and the lead author on the study. "The PLUTO trial shows that we can deliver both intensive behavioral treatment and medications to help people quit by integrating a longitudinal tobacco cessation care program into the lung cancer screening setting."
While further work is needed to identify implementation strategies, researchers recommend that health systems consider integrating longitudinal tobacco cessation care into the lung cancer screen setting in order to improve outcomes for patients who still smoke.
More information: Steven S. Fu et al, Optimizing Longitudinal Tobacco Cessation Treatment in Lung Cancer Screening, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.29903


















