This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
A new article collection on integrating evidence-based programs into clinical practice
As part of its partnership with the Patient-Centered Outcomes Research Institute (PCORI), Medical Care has published its article collection, which provides specific information about the costs that health care systems can expect to incur in promoting the uptake of specific evidence-based programs.
In the September issue, five project teams describe their approaches and methods for determining the costs of implementing programs into routine clinical practice, and they report their cost findings.
"Having cost information available during the decision-making process—before implementation occurs—has been found to be particularly important so that leaders can consider financial implications and weigh trade-offs before investing in implementing an evidence-based practice change," Valerie Lehman, MHA, program officer for dissemination and implementation at PCORI, and colleagues note in an introductory editorial. "Yet information about the cost of implementation is not often available."
Accounting for context-specific considerations when assessing costs of implementation is crucial
One paper in the collections reports on a team that assessed the costs of implementing Connect to Health, an evidence-based pediatric weight management program, into three health care systems that care for pediatric populations with a disproportionately high prevalence of obesity: Denver Health; Prisma Health in Greenville, South Carolina; and Massachusetts General Hospital in Boston.
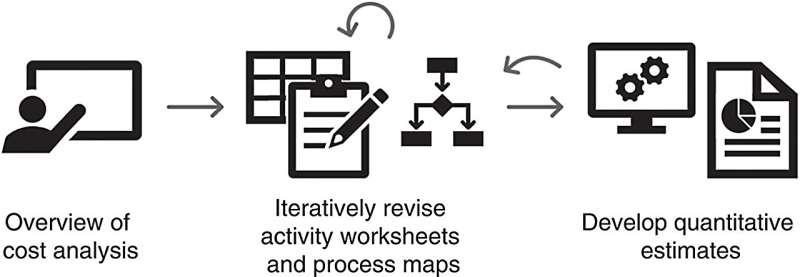
Natalie Smith, Ph.D. and Douglas E. Levy, Ph.D., investigators at the Mongan Institute Health Policy Research Center at Mass General, together with colleagues, used time-driven activity-based costing methods.
Specifically, each of the three sites developed a process map and a detailed report of all implementation actions taken, aligned with major implementation requirements (e.g., electronic health record integration) or strategies (e.g., providing clinician training). For each action, sites identified the personnel involved and estimated the time they spent, and the research team then estimated the total costs of implementation and broke down the costs for major categories of implementation activities.
Process maps showed the program integrated easily into well-child visits. Overall implementation costs ranged from $77,103 to $142,721, with setting up the technological aspects of the program being a major driver of costs. Other drivers included training, engaging stakeholders, and audit and feedback activities, but there was variability across health care systems based on how they chose to implement the program and expend resources.
Site-specific data can be useful to other health care centers
"Beyond just the technological aspects of the program, our findings provide valuable information for future adoption and implementation decisions as they clearly delineate what kinds of costs sites should expect, the personnel involved in various implementation actions, and how costs were distributed across pre-implementation and implementation," Dr. Smith and her co-authors say.
"Disaggregating costs across different categories allows future sites to better plan for what to expect in implementation, even if the exact dollar amounts will likely be different than what was observed in the three research sites."
Ms. Lehman and the other editorialists add that all five papers "provide more information to health care decision-makers on the actual observed costs associated with implementing evidence-based practices. Each team was able to capture the specific types of personnel, as well as the detailed tasks and activities, involved in implementation, essentially laying out clear pathways for future sites considering whether and how to put these evidence-based practices into place."
More information: Smith, Natalie Riva et al, Costs to Implement a Pediatric Weight Management Program Across 3 Distinct Contexts, Medical Care (2023). DOI: 10.1097/MLR.0000000000001891 journals.lww.com/lww-medicalca … t_management.13.aspx




















