This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Researchers take another big step toward HIV cure
Today, HIV can be managed with medical treatment. However, despite 40 years of intensive research, scientists have not yet succeeded in finding a cure for the disease. People with HIV experience a flare-up of the virus only a few weeks after stopping treatment. But now, an international team of researchers, led by scientists at Aarhus University and Aarhus University Hospital, may have moved another step closer to a medication-free existence for the millions living with HIV today.
Last year, the researchers demonstrated that individuals who had just been diagnosed had a stronger immune response against the virus and lower levels of the virus in their blood when they were given so-called monoclonal antibodies against HIV, along with starting regular medical treatment. Monoclonal antibodies against HIV are very specific and highly potent antibodies that are synthetically produced in large quantities and used for experimental treatment.
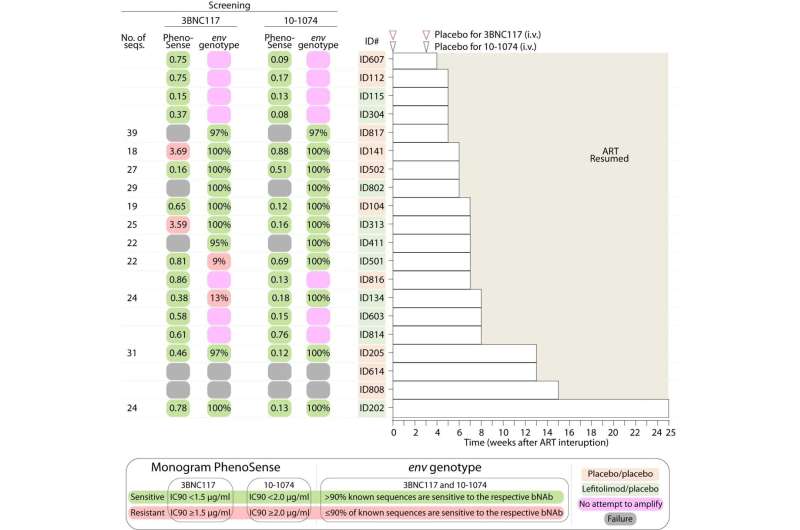
In a new study, recently published in the journal Nature Medicine, the researchers have shown that patients who have been on treatment for years also benefit from this therapy. Specifically, the antibody treatment allows the study participants to suppress the virus for more than three months. While some of the participants continue to spontaneously suppress HIV for more than 18 months after their regular HIV treatment has stopped.
Professor Ole Schmeltz Søgaard from the Department of Clinical Medicine at Aarhus University, is the lead author of the new study and he hopes the new findings will bring us closer to a cure:
"The study is one of the first placebo-controlled trials conducted on humans, where we have shown a way to boost the body's own ability to fight HIV—even when standard treatment is paused. We therefore see the study as an important step towards a cure," he said.
The study was conducted in close collaboration with researchers from Denmark, Norway, Australia, and the U.S..
Antibodies restore immunity
In the trial, study participants from Denmark, Norway, and Australia were randomly divided into four groups. One group received the drug Lefitolimod,designed to enhance immune cell response against the virus, while another group received two monoclonal antibodies (3BNC117 + 10-1074) against HIV, which can eliminate the virus and strengthen the cells' immune system. The third group received standard treatment without experimental medication, while the fourth group received both types of experimental medicine.
And the results of the study are very encouraging, says Dr. Jesper Damsgaard Gunst from Aarhus University Hospital, who is also one of the lead authors of the study:
"Unfortunately, there was no extra benefit from Lefitolimod, but our study shows that people with HIV who receive monoclonal antibodies before pausing their regular HIV medication experience a period of about three months before the virus reappears. Additionally, the immune system in a third of those who received monoclonal antibodies can partially or completely suppress the virus, even after the monoclonal antibodies have left the system," he explained.
Continued need for treatment optimization
Despite the remarkable results of the study, there is still a long way to go before a cure is available, emphasizes Professor Ole Schmeltz Søgaard. First, the researchers need to optimize the treatment and enhance its effects. Therefore, more trials are on the way.
"The hope is that we will gradually improve our experimental treatment strategy to a level where the effect of our treatment is that up to 50%, 70%, or even 100% of patients become medication-free and neither relapse nor can infect others. If we can achieve that, we will have developed a cure for HIV that will change the lives of approximately 38 million people living with the disease today."
The research group is now recruiting participants for a large UK-led clinical trial, which also tests the effectiveness of two monoclonal antibodies against HIV. The group is also planning a larger study across Europe to optimize experimental treatment with monoclonal antibodies.
Ole Søgaard Schmeltz has high expectations for the new trials: "Our hypothesis is that the optimized treatment will have an even stronger effect on both the virus and patients' immunity. In this way, we hope to improve the immune system's ability to permanently suppress the remaining virus in the body."
More information: Jesper D. Gunst et al, Impact of a TLR9 agonist and broadly neutralizing antibodies on HIV-1 persistence: the randomized phase 2a TITAN trial, Nature Medicine (2023). DOI: 10.1038/s41591-023-02547-6





















