This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
A missing piece of the puzzle in a rare life-threatening condition linked to vaccines
A team of scientists led by the University of Aberdeen has taken an important step forward in understanding the mechanisms by which adenovirus-based vaccines, including some of those used in the COVID pandemic, can cause serious adverse reactions.
Working in collaboration with NHS Grampian, NHS Greater Glasgow & Clyde and NHS Lothian, the researchers have identified a new key feature of the ultra-rare condition termed Vaccine Induced Immune Thrombocytopenia and Thrombosis (VITT). This life-threatening condition is associated with the adenovirus-based vaccines to COVID-19, including Oxford-Astra Zeneca and Johnson-Johnson.
During the vaccine rollout, a small number of previously healthy people became rapidly unwell after vaccination and developed sometimes fatal blood clots or bleeding abnormalities. Patients with VITT have unique antibodies to a protein called platelet factor 4 (PF4). The antibodies cause activation of small cell fragments in the blood called, platelets, and trigger blood clotting. In the case of VITT blood clots were often present in unusual sites such as the brain, gut and liver.
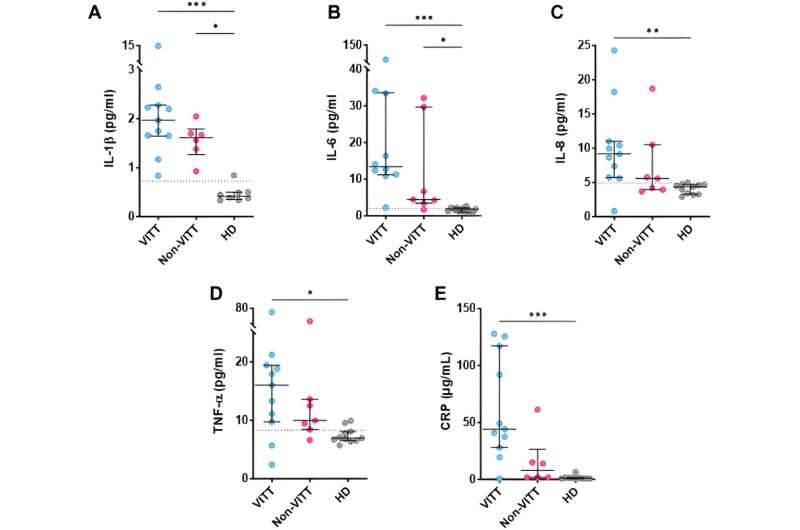
The team led by Professor Nicola Mutch analyzed samples from all suspected cases of VITT from across Scotland. Some of these patients were confirmed to have this rare condition based on the presence of antibodies to PF4 and other clinical features, including the presence of blood clots. Analysis of the samples from these patients found that there was overactivation of the body's natural "blood-clot-busting system," termed fibrinolysis. Uncontrolled fibrinolysis results in breakdown of the main building block of a blood clot, called fibrinogen.
Published in the Journal of Thrombosis and Haemostasis, these important observations help explain both the clot formation and the bleeding complications, commonly intracranial hemorrhage, seen in VITT patients.
This missing piece of the puzzle is vital, as adenoviruses are used in other aspects of medicine, including as vectors in gene therapy for cancers and hemophilia. Understanding the mechanisms by which adenovirus-based products can cause adverse reactions, like VITT, is crucial in considering future use in other medicinal products. It may also guide therapeutic strategies to treat similar conditions to VITT in the future.
In this study, all samples from suspected cases of VITT seen in Scottish hospitals were included in the analysis. This allowed the team to make comparisons between patients with a VITT diagnosis and those initially suspected but who were ultimately found to be negative for the condition. Patients with VITT showed a very high incidence of a complication called disseminated intravascular coagulation (DIC), a severe abnormality in the blood clotting cascade which can cause organ damage and uncontrollable bleeding. In patients with VITT there was also evidence of excessive breakdown of these blood clots and their precursor, fibrinogen, suggesting overactivation of fibrinolysis.
Emeritus Professor, Henry Watson explains, "This research was triggered by the recognition of the catastrophic outcomes of VITT, in which previously healthy, frequently young individuals were becoming rapidly unwell. This extremely rare but often fatal reaction to the adenovirus-based COVID-19 vaccine usually occurred around seven to 30 days after vaccination.
"Given that Aberdeen held all of the Scottish samples of suspected VITT, we quickly realized this was a unique opportunity to help define the features of this complex syndrome and how it differs from other thrombotic conditions."
Professor Mutch adds, "Our work identifies a novel aspect of VITT which was previously unrecognized. It helps us to understand the mechanisms underlying the clinical observations, whereby the patients suffer from complications due to both blood clots and bleeding at the same time.
"The demonstration of overt disseminated intravascular coagulation and the breakdown of the clotting protein fibrinogen in VITT had not previously been recognized but this helps explain the acute symptoms and rapid course of this extremely rare complication of vaccination with adenovirus-based vaccines."
More information: Megan Simpson et al, Fibrinogenolysis and fibrinolysis in vaccine-induced immune thrombocytopenia and thrombosis, Journal of Thrombosis and Haemostasis (2023). DOI: 10.1016/j.jtha.2023.09.007





















