This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
proofread
Mozambique faces alarming multidrug-resistant tuberculosis epidemic
With one of the highest tuberculosis (TB) incidences (368 cases/100,000 population) in the African region, Mozambique is particularly affected by the TB epidemic. Drug-resistant TB is also a major problem, with 4,800 new cases of multidrug resistant (MDR)/rifampicin-resistant TB in the country estimated in 2021.
Even more worrisome, researchers from an international consortium found a high proportion of fluoroquinolone resistance and increasing resistance to bedaquiline among MDR-TB strains, two key drugs in treatment regimens currently used to treat MDR-TB patients.
In addition, the researchers documented the spread of "diagnostic escape" MDR-TB strains, carrying a rifampicin resistance mutation that cannot be detected by rapid molecular diagnostic tests currently in widespread use. The results of this study have now been published in The Lancet Infectious Diseases.
Effective diagnostics and treatment of patients affected by MDR-TB are key for TB control. In Mozambique and other African countries, the WHO has recommended nationwide use of the Xpert MTB/RIF Ultra test as a first line diagnostic test for MDR-TB to guide rapid MDR-TB treatment in line with the latest World Health Organization (WHO) guidelines.
Recently, the WHO recommended a new 6-month oral treatment regimen (BPaLM) composed of bedaquiline, pretomanid and linezolid plus moxifloxacin (in the absence of fluoroquinolone resistance) for the treatment of patients with MDR-TB. Although this regimen holds great promise, the emergence of fluoroquinolone and/or bedaquiline resistance described recently will threaten the success and longevity of the regimen.
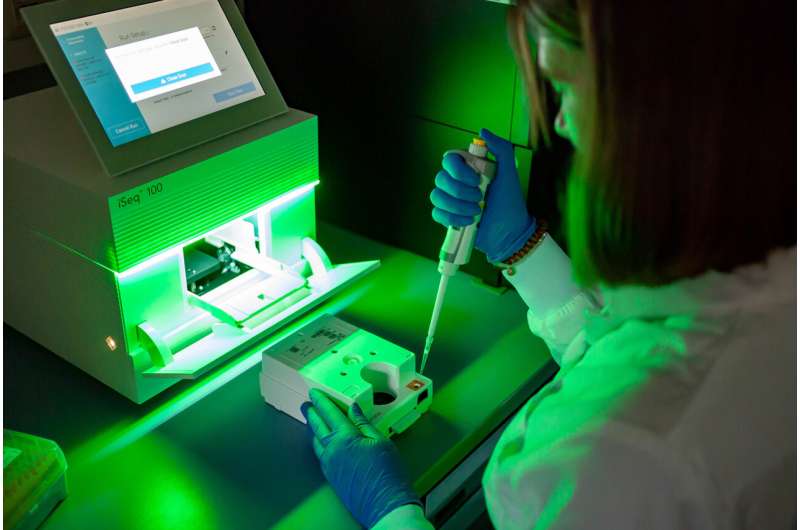
In this study, led by scientists from the Research Center Borstel, Leibniz Lung Center and the National Institute of Health (Instituto Nacional de Saúde, INS, Mozambique), researchers used cutting-edge genomic sequencing technology on a set of rifampicin resistant (RR) Mycobacterium tuberculosis (Mtb) strains submitted to the National Tuberculosis Reference Laboratory in Maputo between 2015 and 2021 to study the transmission and evolution of drug resistant Mtb strains over time.
It has been found that more than 20% of the MDR Mtb strains in Mozambique already exhibit fluoroquinolone. Further, bedaquiline resistance is steadily increasing, from 3% in 2016 to 14% in 2021 among the MDR/RR Mtb strains. The data also indicate a high rate of recent transmission, especially of Mtb strains with high levels of drug resistance, such as pre-XDR or XDR strains.
"The rapid evolution of resistance and the efficient transmission of highly resistant M. tuberculosis strains represent a major threat to TB control in Mozambique and the neighbor regions," says Prof. Niemann, study coordinator at the Research Center Borstel, and PI at the Leibniz Science Campus EvoLUNG, the Cluster of Excellence "Precision Medicine in Chronic Inflammation" (PMI) and the German Center for Infection Research (DZIF).
Equally worrisome is the spread of Mtb strains with a particular rifampicin resistance mutation (I491F), which was not detected by Xpert MTB/RIF Ultra and commercially available line probe assays. A large proportion of the I491F strains have a further resistance to bedaquiline, or even combined resistances to bedaquiline and fluoroquinolone. Comparison with strains from South Africa and Eswatini supports the cross border spread of I491F strains, a finding, that needs to be urgently investigated.
"Given the current diagnostic algorithms and treatment regimens, both, the emergence of rifampicin resistance due to I491F strains and bedaquiline resistance in general, may jeopardize efforts to contain the drug resistant TB epidemic in Mozambique," says Dr. Sofia Viegas, lead scientist and deputy general director at INS.
In a more general context, the study raises fundamental points regarding the development and introduction of new anti-TB agents or regimens. In the absence of effective diagnostics and direct translation of results into clinical decisions and resistance-adapted drug regimens, there is a high risk of rapid development of resistance, rendering newly developed medicines ineffective within a short timeframe.
The study also calls into question the role of rapid molecular tests such as Xpert MTB/RIF in regions where the prevalence of "diagnostic escape" strains is high. The uncontrolled transmission of MDR Mtb strains in Mozambique and other parts of Africa represents a tremendous challenge for the fight against TB in the 21st century, and underlines the importance of effective diagnosis and TB surveillance based on comprehensive molecular methods such as sequencing technologies.
"Our research focuses on these topics, which we work on in national and international projects. Here, the translation of the basic research results into application is of particular importance," explains Prof. Niemann.
More information: Ivan Barilar et al, Emergence of bedaquiline-resistant tuberculosis and of multidrug-resistant and extensively drug-resistant Mycobacterium tuberculosis strains with rpoB Ile491Phe mutation not detected by Xpert MTB/RIF in Mozambique: a retrospective observational study, The Lancet Infectious Diseases (2023). DOI: 10.1016/S1473-3099(23)00498-X





















