This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Under-the-skin implant could treat type I diabetes
A collaboration between researchers from Cornell and University of Alberta, Edmonton, has created a new technique to treat type 1 diabetes: implanting a device inside a pocket under the skin that can secrete insulin while avoiding the immunosuppression that typically stymies management of the disease.
The approach would offer an easier, long-term and less invasive alternative to insulin injections or traditional transplants that require immunosuppression.
The group's paper is published in Nature Biomedical Engineering.
For the last decade, Minglin Ma, professor of biological and environmental engineering at Cornell, has been trying to develop a better way to control the disease.
In 2017, he unveiled a removeable polymer thread containing thousands of islet cells, protected by a thin hydrogel coating, that could be implanted in a patient's abdomen. The enclosed islets could secrete insulin in response to the body's diminished blood-sugar levels while also receiving a steady flow of nutrients and oxygen to stay healthy. Ma's lab created a more robust version in 2021 that proved effective in controlling blood sugar in diabetic mice for up to six months.
Those projects prompted James Shapiro of the University of Alberta, Edmonton, to reach out about a possible collaboration. Shapiro had created a method for inserting islets in channels just under a person's skin, then applying immunosuppression to protect them.
"I was intrigued by the virtue of Ma's approach as it avoided the need for immunosuppression, and I wondered if we might combine our two innovative strategies to improve cell survival," Shapiro said. "Indeed it worked."
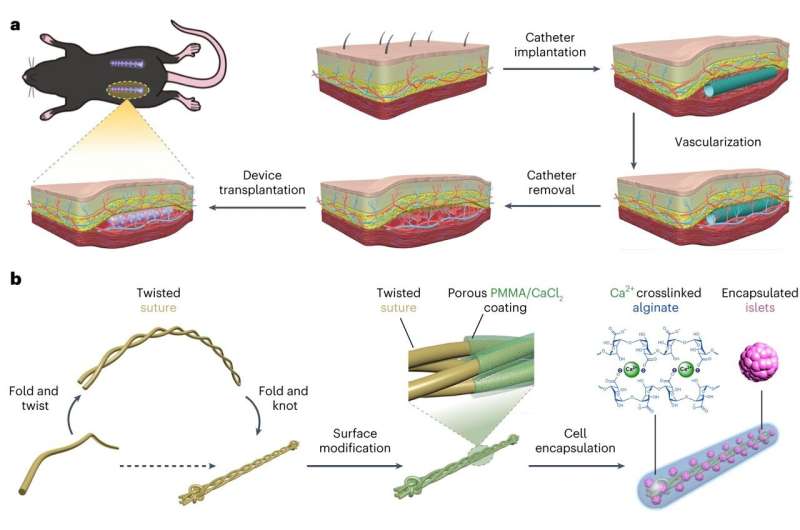
The resulting new system is named SHEATH (Subcutaneous Host-Enabled Alginate THread).
The installation is a two-step process. First, a series of nylon catheters are inserted under the skin, where they remain for four to six weeks—long enough for blood vessels to form around the catheters. When the catheters are removed, the islet devices, which are approximately 10 centimeters long, are inserted into the pocket of space the catheters created, and the surrounding vascular system remains intact.
"That channel is a perfect fit for our device," Ma said. "Putting something under your skin is much easier, much less invasive than in the abdomen. It can be done as an outpatient procedure, so you don't have to stay in the hospital. It can be done under local anesthesia."
While additional challenges for the long-term clinical application of the device remain, Ma is hopeful that future versions will be able to last for two to five years before needing to be replaced.
"The challenge is, it's very difficult to keep these islets functional for a long time inside of the body where you have a device, because the device blocks the blood vessels, but the native islet cells in the body are known to be in direct contact with vessels that provide nutrients and oxygen," Ma said. "The device is designed in a way that we can maximize the mass exchange of nutrients and oxygen, but we may need to provide additional means to support the cells for a long-term function."
More information: Long-Hai Wang et al, Inflammation-induced subcutaneous neovascularization for the long-term survival of encapsulated islets without immunosuppression, Nature Biomedical Engineering (2023). DOI: 10.1038/s41551-023-01145-8




















