This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New 3D bioprinted model to study common liver disease, find effective treatment
Metabolic dysfunction-associated steatohepatitis, or MASH, is an inflammatory, liver-scarring disease that has reached epidemic proportions, with an estimated 1.5% to 6.5% of U.S. adults afflicted by the condition, and roughly 24% of adults having nonalcoholic fatty liver disease (NAFLD).
MASH, previously known as nonalcoholic steatohepatitis or NASH, is a more serious complication of NAFLD, now called metabolic dysfunction–associated steatotic liver disease or MASLD. The nomenclature changed recently to reduce the stigma attached to the older terms. Neither disease is associated with alcohol consumption.
There are no approved pharmacological therapies for MASH, in part due to a lack of adequate preclinical models for study and testing. A new paper published in The American Journal of Pathology from researchers at Sanford Burnham Prebys, with colleagues at Viscient Biosciences, a San Diego–based biotech, and UC San Diego and Salk Institute, describes a 3D bioprinted liver tissue model employing liver cells from healthy or MASH-diseased donors.
Senior and corresponding study author David A. Brenner, MD, president and CEO of Sanford Burnham Prebys and a longtime leader in liver disease research, said, "These tissues display all of the characteristics of MASH, including fibrosis, without any additional disease-inducing agents."
Co-author Jeffrey Miner, Ph.D., cofounder and chief scientific officer of Viscient Biosciences, underscored the importance of being able to produce a high fidelity in vitro human primary cell model of MASH. "This approach utilizes the patient's own diseased cells, allowing them to generate the disease within the bioprinted tissue. We specifically exclude agents that artificially induce disease. We believe this advance enhances the translation of our results to human clinical trials and drug discovery."
Researchers were able to create their model by layering a mix of primary liver cells and supporting non-parenchymal liver cells (hepatic stellate, liver sinusoidal endothelial, and Kupffer) to create bioprinted 3D tissues derived from patient cells.
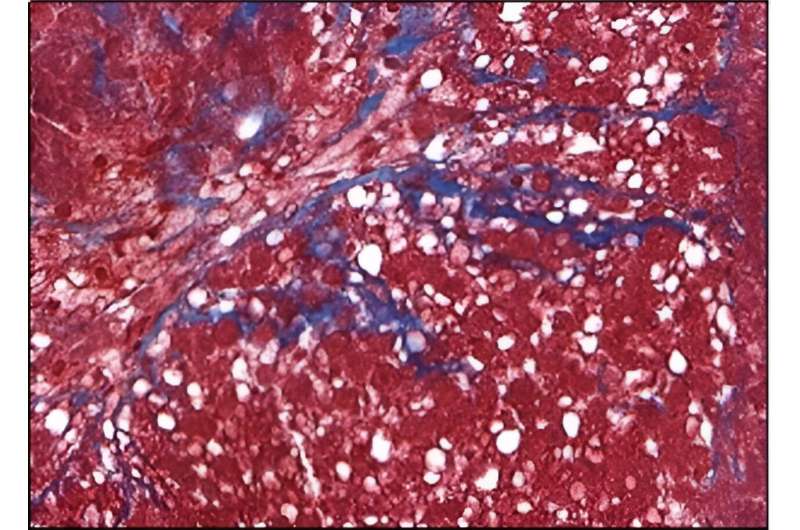
Notably, the resulting diseased tissues displayed fibrosis, an abnormal accumulation of collagen that in the liver, results in progressive scarring and dysfunction, leading to cirrhosis and liver cancer. With no way to stop or reverse fibrosis, the only recourse is an organ transplant.
The new models offered a peek at the underlying pathology, illuminating the roles of hepatic stellate and liver sinusoidal endothelial cells in the disease process.
Dr. Miner said, "This model represents a fully human system with the potential to detect clinically active targets and therapies. That's important given that current discovery and animal models have not translated into any approved drugs."
More information: Philip K. Tan et al, Role of Hepatic Stellate and Liver Sinusoidal Endothelial Cells in a Human Primary Cell Three-Dimensional Model of Nonalcoholic Steatohepatitis, The American Journal of Pathology (2023). DOI: 10.1016/j.ajpath.2023.12.005



















