This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Thinning of brain region may signal dementia risk 5–10 years before symptoms
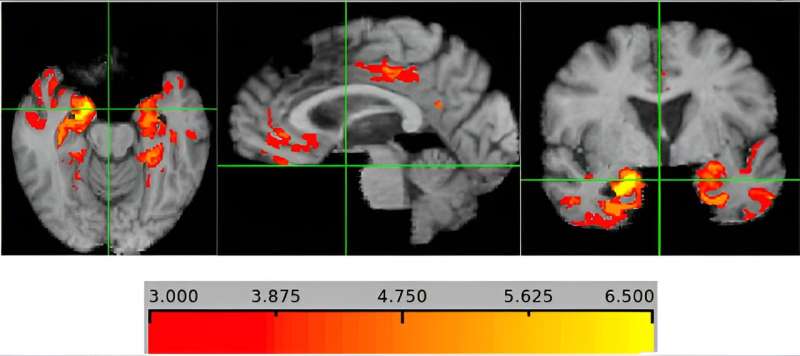
A ribbon of brain tissue called cortical gray matter grows thinner in people who go on to develop dementia, and this appears to be an accurate biomarker of the disease five to 10 years before symptoms appear, researchers from The University of Texas Health Science Center at San Antonio (also called UT Health San Antonio) report.
The researchers, working with colleagues from The University of California, Davis, and Boston University, conducted an MRI brain imaging study published in Alzheimer's & Dementia. They studied 1,000 Massachusetts participants in the Framingham Heart Study and 500 people from a California cohort. The California volunteers included 44% representation of Black and Hispanic participants, whereas the Massachusetts cohort was predominantly non-Hispanic white. Both cohorts were 70 to 74 years of age on average at the time of MRI studies.
"The big interest in this paper is that if we can replicate it in additional samples, cortical gray matter thickness will be a marker we can use to identify people at high risk of dementia," said study lead author Claudia Satizabal, Ph.D., of UT Health San Antonio's Glenn Biggs Institute for Alzheimer's and Neurodegenerative Diseases. "By detecting the disease early, we are in a better time window for therapeutic interventions and lifestyle modifications, and to do better tracking of brain health to decrease individuals' progression to dementia."
Repeating the Framingham findings in the more-diverse California cohort "gives us confidence that our results are robust," Satizabal said.
Sifting MRIs for a pattern
While dementias can affect different brain regions, Alzheimer's disease and frontotemporal dementia impact the cortex, and Alzheimer's is the most common type of dementia.
The study compared participants with and without dementia at the time of MRI. "We went back and examined the brain MRIs done 10 years earlier, and then we mixed them up to see if we could discern a pattern that reliably distinguished those who later developed dementia from those who did not," said co-author Sudha Seshadri, MD, director of the Glenn Biggs Institute at UT Health San Antonio and senior investigator with the Framingham Heart Study.
"This kind of study is only possible when you have longitudinal follow-up over many years as we did at Framingham, and as we are building in San Antonio," Seshadri said. "The people who had the research MRI scans while they were well and kept coming back to be studied are the selfless heroes who make such valuable discoveries, such prediction tools, possible."
The results were consistent across populations. Thicker ribbons correlated with better outcomes and thinner ribbons with worse, in general. "Although more studies are needed to validate this biomarker, we're off to a good start," Satizabal said. "The relationship between thinning and dementia risk behaved the same way in different races and ethnic groups."
Clinical trial researchers could use the thinning biomarker to minimize cost by selecting participants who haven't yet developed any disease but are on track for it, Seshadri said. They would be at greatest need to try investigational medications, she said.
The biomarker would also be useful to develop and evaluate therapeutics, Seshadri noted.
Future directions
Satizabal said the team plans to explore risk factors that may be related to the thinning. These include cardiovascular risk factors, diet, genetics and exposure to environmental pollutants, she said.
"We looked at APOE4, which is a main genetic factor related to dementia, and it was not related to gray matter thickness at all," Satizabal said. "We think this is good, because if thickness is not genetically determined, then there are modifiable factors such as diet and exercise that can influence it."
Could the MRI gray matter biomarker be used widely someday?
"A high proportion of people going to the neurologist get their MRI done, so this thickness value might be something that a neuroradiologist derives," Seshadri said. "A person's gray matter thickness might be analyzed as a percentile of the thickness of healthy people for that age."
More information: Claudia L. Satizabal et al, A novel neuroimaging signature for ADRD risk stratification in the community, Alzheimer's & Dementia (2023). DOI: 10.1002/alz.13600





















