This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Cytometry chip supports new revolution in cancer care for a truly personalized treatment plan
Imec teamed up with the KU Leuven laboratory of tumor immunology and immunotherapy for the first clinical validation of its cell sorter chip technology. The chip successfully identified PD-1 positive T cells in the blood samples of 15 ovarian cancer patients, matching the accuracy of the established gold standard in cytometry—bulky and costly flow cytometry instruments like FACS. The work has been publsihed in Cells.
This is the first step in developing a point-of-care tool for immune profiling, a cutting-edge development in cancer therapy aimed at tailoring patient-specific treatment plans.
First use of cell sorter technology in a clinical setting
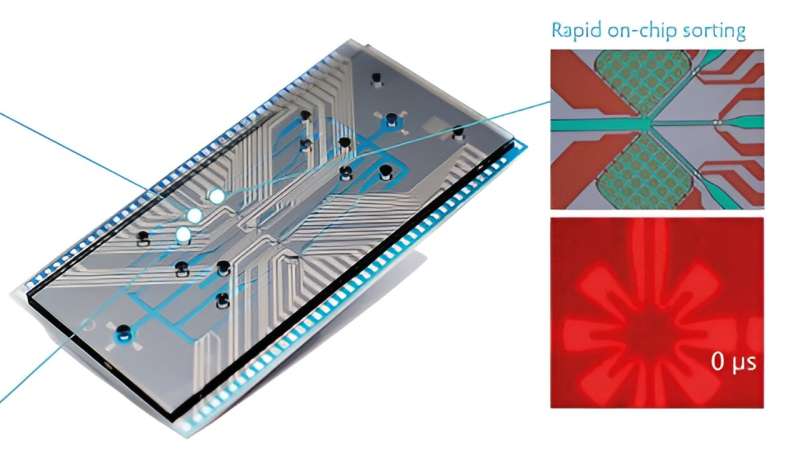
Imec's cytometry and cell sorter technology uses microfluidic channels on-chip to guide a sample with fluorescently labeled cells towards an excitation laser, a detection unit, and a sorting junction where the target cells are pushed into a side channel. This 'pushing' is done by means of vapor bubbles that are created in a water-filled microchamber with microheaters. At the end of this fluidic side channel, the target cells can be collected and quantified.
These chips were tested in a setting using patient samples, at imec, and in the laboratory of tumor immunology and immunotherapy of KU Leuven, respectively. "We demonstrated that this fluidics chip can be used to detect a specific kind of immune cell (CD8+PD-1+ T-cells), as effectively as a conventional flow cytometer tool," explains Ann Vankerckhoven, former Ph.D. student at Coosemans' lab.
Immune profiling for better cancer treatment
"The more we understand the immune system, the clearer it becomes that it is important to monitor the response of the immune system during disease and treatment," says professor An Coosemans, expert in tumor immunology & immunotherapy for ovarian cancer.
"It's for this reason that we use flow cytometry tools in our lab to do immune profiling—the identification and quantification of a patient's immune cells at a certain point in time. It is interesting information to decide on the most effective treatment for a cancer patient. And by doing this profiling during the treatment, we gain insights into the effectiveness of the treatment. In this way, it's a monitoring tool to guide therapy."
"Even though this immune profiling for therapy guidance is a very promising new area in cancer research and treatment, it is not used in clinical practice because the flow cytometry equipment is expensive, bulky, and complex to use. It is only available in centralized dedicated labs, so blood samples would need to be transported, which takes time and special transport requirements to keep the cells alive. It is therefore difficult to use this to routinely monitor the patient," says Coosemans.
A point-of-care tool for immune profiling
"With imec's cell sorter technology, we can provide oncologists with a portable tool—the size of a lunchbox—that can be used in an oncologist's office or daycare center to check a patient's immune system condition at different time points," explains Liesbet Lagae, imec fellow and inventor of the cell sorter concept.
"The sample would be a drop of blood and by inserting the chip cartridge into an analyzing desktop tool, the parameters could be read out within a few minutes. Because the chip is made with standard chip technology—on 200mm silicon wafers—it can be mass-produced at a reasonable cost. This means that it can be disposable if needed, preventing cross-sample contamination."
"Also, the chip fabrication process allows to make tens of microfluidic channels per chip. It's this level of parallelization that holds the potential for achieving high throughput without losing sensitivity (and thus a very fast time to result, say 10 minutes for a complete immune signature). By comparing immune signatures to larger datasets, oncologists will immediately know if the therapeutic effect is being reached."
PD-1, a key protein in guiding cancer treatment
"We wanted to investigate whether imec's cell sorter concept could identify and quantify immune cells as effectively as our flow cytometry equipment," adds Coosemans.
"For our proof-of-concept experiments, we selected the CD8+PD-1+ T cell. This specific T cell exhibits both CD8 and PD-1 proteins on its surface. The presence of the CD8 protein identifies these cells as cytotoxic T cells, which play a crucial role in recognizing and eliminating targets such as cancer cells."
PD-1 stands for programmed cell death protein 1. Its primary function is to inhibit or regulate the activity of T cells. When PD-1 interacts with its ligands (PD-L1 or PD-L2), it delivers inhibitory signals to the T cell and prevents excessive immune responses. Put simply, it allows the immune system to come back 'into balance' once a foreign invader has been successfully attacked.
However, cancer cells can exploit this pathway by overexpressing PD-1 ligands, thereby suppressing the immune response. As a consequence, cancer cells can grow without being stopped.
By looking at PD-1 positive T cells in the blood of a cancer patient, the oncologist gets for example an indication of whether or not the cancer is using the above immune-evading strategy. In this case, it can be a good idea to use so-called immune checkpoint inhibitor drugs that 'protect' the PD-1 proteins on T cells from binding with the PD-1 ligands produced by the tumor cells. T cells regain their function and can again destroy them.
"For this study we used blood samples from 15 patients with ovarian cancer from the gynecology department of the University Hospitals Leuven, headed by professor Dirk Timmerman. Patients were of different ages and in different stages of disease progression," explains Coosemans.
"The heterogeneity of the group is important to demonstrate the reliability of the test. PD-1 is present in very small amounts, so it's a very 'weak' marker, present in different concentrations depending on the patient, the progression of the disease, the treatment plan, etc."
Further development to unlock full potential
Coosemans emphasizes the importance of further developing this point-of-care test for immune profiling. "With cancer, you don't want to lose precious time by giving the patient an expensive therapy that doesn't work. This is certainly true for ovarian cancer. This kind of cancer is mostly detected at a very late stage because the tumor has a lot of 'free' space to grow in the abdominal cavity before the patient will experience this as pain."
"Imec's cell sorter technology has the potential to provide oncologists with a tool to do initial and repeated immune profiling to choose the most effective treatment."
"For now, we have demonstrated the effectivity of the fluidic part," explains imec project manager Sarah Libbrecht. "The next step is to integrate the photonic part, with multiple lasers to excite the fluorescent labels and collect the signature on a detector array. Imec's silicon nitride photonics platform is ideally suited for this."
"It was wonderful to see our cell-sorter technology being used in a clinically-relevant project that could change people's lives," concludes Lagae.
"It's furthermore useful in so many application fields, ranging from proteomics to cell and gene therapy (CGT). On the latter, we are today actively partnering with industry to reduce the cost and complexity of CGT manufacturing. For example, we are using the same cell sorter platform in a collaboration with Austrian technology startup Sarcura to develop automated T cell separation for use in CGT manufacturing."
"And next to industry, we also partner with clinical practice—as was proven in this project—to demonstrate the cell sorter's potential as a tool to better understand diseases and to set up new kinds of diagnostic or therapeutic devices for personalized medicine and therapy monitoring. In this way, the same chip technology can solve two enormous challenges in cancer care—the cost and personalization of therapy."
More information: Sarah Libbrecht et al, A Microfluidics Approach for Ovarian Cancer Immune Monitoring in an Outpatient Setting, Cells (2023). DOI: 10.3390/cells13010007


















