This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Europe-wide study finds gut microbiota predict severity of acute pancreatitis
In a Europe-wide study involving 15 pancreas centers, researchers at the University Medical Center Göttingen (UMG) have discovered that the microbial composition of the gut, the gut microbiome, influences the course of severe acute pancreatitis. Based on the changes in the gut microbiome, a model was developed to predict the severity of pancreatitis. The results could contribute to new treatment strategies. The study is published in Gut.
Severe acute pancreatitis is a life-threatening disease that requires highly specialized multidisciplinary treatment. It is often triggered by gallstone disease or increased alcohol consumption. In rare cases, medication, lipometabolic disorders, autoimmune or viral diseases can also be the cause.
In most cases, the extremely painful disease is mild and patients can be discharged from hospital after a few days. In about 20% of cases, however, the course is severe and potentially life-threatening, with organ failure and complications such as internal bleeding caused by the destruction of organs or blood vessels due to inflammation.
Triggering factors and mechanisms for a severe course of the disease are not yet sufficiently clarified, which means that no therapeutic approaches can be applied in the early phase of the disease that could have a decisive influence on the course and severity of the disease.
Junior researcher Dr. Christoph Ammer-Herrmenau and senior physician Prof. Neesse, MD, Ph.D., both working in the Department of Gastroenterology, Gastrointestinal Oncology and Endocrinology at the University Medical Center Göttingen (UMG), have investigated the role of the gut microbiome, a complex community of trillions of microorganisms, in connection with the severity of acute pancreatitis in a Europe-wide trial involving 15 pancreas centers.
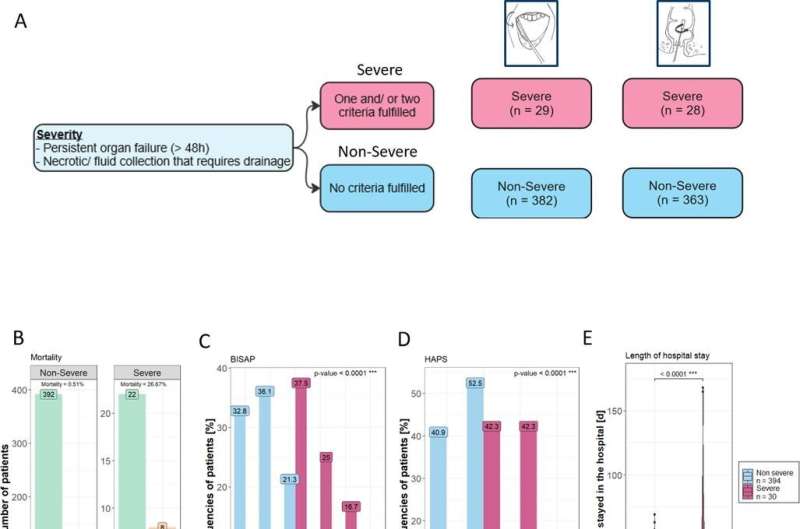
Based on the changes in the microbiome in 424 patients with acute pancreatitis, a prediction model was developed that outperformed previously used prediction scores for the severity of the disease. The results show that early changes in the gut microbiome are clearly associated with the later severity of acute pancreatitis, mortality and the length of hospitalization of patients.
Further bioinformatic analyses also showed that microbial short-chain fatty acids may play an important role in the development of severe, life-threatening pancreatitis.
Healthy humans are colonized by numerous microbes. Trillions of bacteria can be detected in the gastrointestinal tract alone. The microorganisms and their metabolic products influence numerous processes and functions as well as inflammatory and immunoregulatory processes in the human body.
For the study, the gut microbiome of 424 patients with acute pancreatitis was analyzed from oral and rectal swabs and correlated with the subsequent course of the disease, the length of hospital stay and the mortality of the patients. Various confounding factors influencing the microbiome were included in the investigations, such as age, gender, nicotine consumption and the use of antibiotics.
"In order to investigate the potential influence of the gut microbiome on the severity and course of acute pancreatitis, we took swabs from the mouth and rectum of patients in the emergency room. The microbial composition of the samples was then determined on the basis of the genetic material, the DNA, using Oxford nanopore sequencing, which allows long DNA fragments to be analyzed completely. With the help of subsequent bioinformatic methods, it is possible to precisely identify the bacteria down to species level," says Dr. Christoph Ammer-Herrmenau, first author of the study.
"Our results show a highly significant change in the gut microbiome in patients who later developed a severe form of pancreatitis, had to stay in hospital longer or even died. Thus, the microbial composition of the gut can predict the course of the disease at an early stage, however, there is currently no proof that these changes in the microbiome actually trigger the severe course of the disease.
"The patterns of metabolic pathways that we were able to identify using bioinformatic prediction models are intriguing and provide initial indications that short-chain fatty acids produced by microorganisms may have an influence on pancreatic inflammation," says Dr. Ammer-Herrmenau.
"We will investigate these promising results in a follow-up study together with our national and international partners in order to translate the new findings into new treatment strategies for our patients as soon as possible," says research group leader Prof. Neesse, MD, Ph.D.
More information: Christoph Ammer-Herrmenau et al, Gut microbiota predicts severity and reveals novel metabolic signatures in acute pancreatitis, Gut (2023). DOI: 10.1136/gutjnl-2023-330987



















