This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Fixing rogue brain cells may hold key to preventing neurodegeneration
A team led by scientists at the Case Western Reserve University School of Medicine has identified a new therapeutic approach for combating neurodegenerative diseases, offering hope of improved treatments for Alzheimer's disease, Parkinson's disease, Vanishing White Matter disease, and multiple sclerosis, among others.
Neurodegenerative diseases, which affect millions of people worldwide, occur when nerve cells in the brain or nervous system lose function over time and ultimately die, according to the National Institutes of Health. Alzheimer's disease and Parkinson's disease are the most common.
The research team's new study, published in the journal Nature Neuroscience, focused on astrocytes—the brain's most abundant cells, which normally support healthy brain function. Growing evidence indicates astrocytes can switch to a harmful state that increases nerve-cell loss in neurodegenerative diseases.
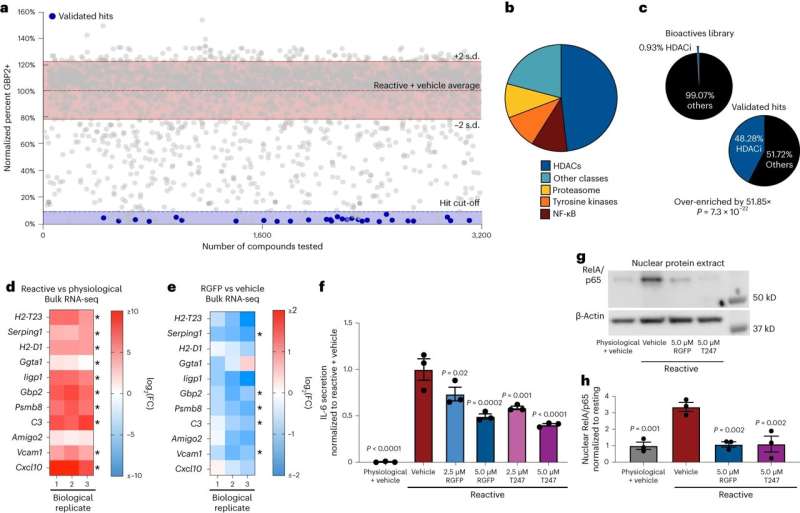
The researchers created a new cellular technique to test thousands of possible medications for their ability to prevent these rogue astrocytes from forming.
"By harnessing the power of high-throughput drug screening, we've identified a key protein regulator that, when inhibited, can prevent the formation of harmful astrocytes," said Benjamin Clayton, lead author and National Multiple Sclerosis Society career transition fellow in the laboratory of Paul Tesar at the Case Western Reserve School of Medicine.
They found that blocking the activity of a particular protein called HDAC3 may prevent the development of dangerous astrocytes. The scientists discovered that by administering medications that specifically target HDAC3, they were able to prevent the development of dangerous astrocytes and significantly increase the survival of nerve cells in mouse models.
"This research establishes a platform for discovering therapies to control diseased astrocytes and highlights the therapeutic potential of regulating astrocyte states to treat neurodegenerative diseases," said Tesar, the Dr. Donald and Ruth Weber Goodman Professor of Innovative Therapeutics and the study's principal investigator.
Tesar, also director of the School of Medicine's Institute for Glial Sciences, said more research needs to be done before patients might benefit from the promising approach. But, he said, their findings could lead to the creation of novel therapies that disarm harmful astrocytes and support neuroprotection—perhaps improving the lives of people with neurodegenerative illnesses in the future.
"Therapies for neurodegenerative disease typically target the nerve cells directly," Tesar said, "but here we asked if fixing the damaging effects of astrocytes could provide therapeutic benefit. Our findings redefine the landscape of neurodegenerative disease treatment and open the door to a new era of astrocyte targeting medicines."
More information: Benjamin L. L. Clayton et al, A phenotypic screening platform for identifying chemical modulators of astrocyte reactivity, Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01580-z



















