This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Exploring why some newborns develop severe infections
Compared to adults, newborns are highly susceptible to infections and these infections can cause serious health complications and even death.
One factor known to affect a newborn's response to infection is a condition called neonatal neutropenia, in which the infant fails to make enough neutrophils, the immune system's first responders. What underlies this immune deficiency, which greatly increases a newborn's susceptibility to infection, is largely unknown, leaving clinicians with little understanding of how to prevent or treat it.
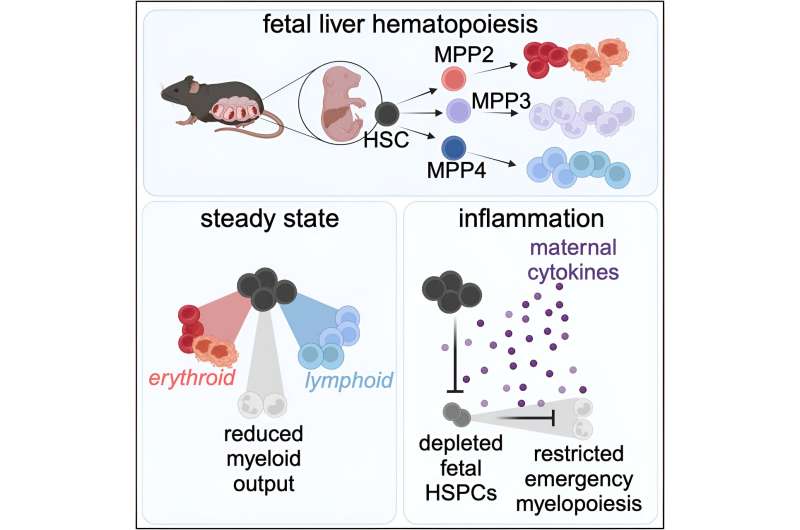
A new study of mice by Columbia University researchers now suggests that many cases of neonatal neutropenia may originate from suppression of the fetus's blood-forming stem cells, a natural maternal mechanism that protects the placenta from inflammation but may leave newborns vulnerable to infection if not turned off after birth.
"We still have much to learn about neonatal neutropenia, but this is an encouraging step forward in developing new treatments. Our findings tell us that it may be more productive to counteract maternal factors that suppress fetal and neonatal hematopoietic stem cells, instead of trying to directly boost the output of these cells," says study leader Emmanuelle Passegué, Ph.D., Alumni Professor of Genetics & Development at the Vagelos College of Physicians and Surgeons and director of the Columbia Stem Cell Initiative at Columbia University.
The clinical challenge
Infants with neonatal neutropenia can develop early-onset sepsis, a life-threatening infection, in the first 72 hours of life.
"Early sepsis is a big problem in full-term infants, but it's even more dangerous for preterm infants and mortality for these infants is very high," says first author Amélie Collins, MD, Ph.D., assistant professor of pediatrics and a neonatologist who treats these hospitalized infants.
Doctors use broad-spectrum antibiotics to treat infants with early-onset sepsis, but antibiotics aren't always enough and often produce other complications. "A treatment that boosts these infants' immune system could have a big impact," Collins says.
The prevailing theory of neonatal neutropenia is that fetuses and neonates with the condition lack the regenerative capacity to produce large numbers of neutrophils to fight infection.
"But what that actually means from a mechanistic standpoint has been unknown," Collins says. "Perinatal hematopoiesis has been an understudied area of biology."
Experiments and results
To understand how neutropenia develops in infants, Collins and Passegué used mouse models to investigate how fetal and neonatal hematopoietic stem cells respond to infection.
Adults with infections usually rely on emergency myelopoiesis, a rapid-response mechanism of hematopoietic stem cells that generates large numbers of immune cells, including neutrophils.
Collins and Passegué found that although emergency myelopoiesis becomes functional early in fetal development—the fetus's hematopoietic stem cells are capable of making neutrophils—the fetus does not turn it on.
That suggested an external factor suppresses fetal myelopoiesis, so the researchers then searched for and found a maternal factor—interleukin 10 or IL-10—that prevents emergency myelopoiesis from being activated during fetal development. Collins and Passegué found that the absence of IL-10 can restore emergency myelopoiesis in the fetus and boost neonatal neutrophil production in a manner that is likely to have important clinical benefits.
"This is the key translational advance of our study," says Collins. "Now that we know fetal and neonatal stem cells can produce neutrophils and we've identified IL-10 as one of the factors that suppress emergency myelopoiesis, we should be able to understand the mechanism and find places where we can intervene."
Potential impact and future directions
The discovery was also made possible with a second mouse model developed by the researchers that allowed them to track what happens in mouse pups after they're born (because removing IL-10 comes at the cost of fetal demise in infected pregnant mice).
This second model showed that newborn pups can engage emergency myelopoiesis pathways after they are born and will be crucial for future studies.
"We are now able to learn more about how maternal IL-10 suppresses fetal hematopoietic stem cells and what signals remove the restraints after birth to turn these exciting findings into an effective therapy," says Passegué.
The paper is published in the journal Cell.
More information: Amélie Collins et al, Maternal inflammation regulates fetal emergency myelopoiesis, Cell (2024). DOI: 10.1016/j.cell.2024.02.002




















