This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Multiple biomaterials for immediate implant placement tissue repair: Current status and future perspectives
A study published in the journal MedComm – Biomaterials and Applications, led by Dr. Xiaojing Wang from the Department of Oral Implantology at The Affiliated Hospital of Qingdao University, focuses on addressing tooth loss, a prevalent dental condition linked to accidents, decay, periodontal disease, and congenital deficiencies.
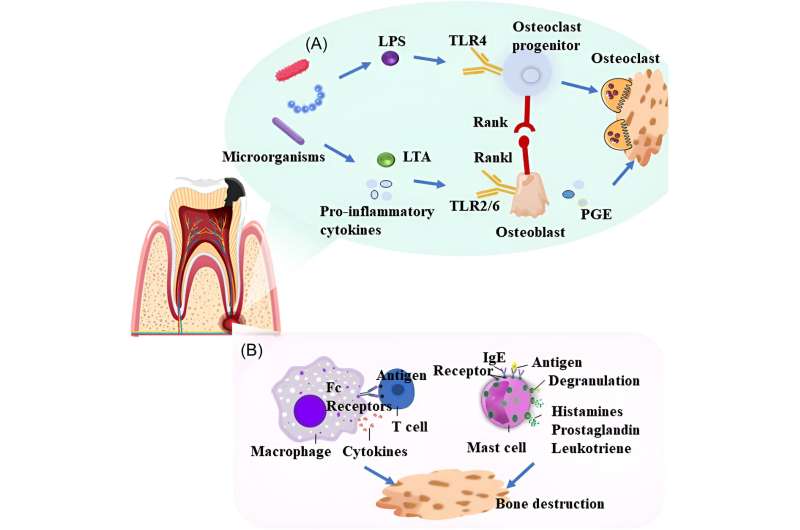
The role of microorganisms and their metabolites is critical in the development and progression of periapical and periodontal lesions, as they can directly damage tissue cells or induce damage through inflammatory and immune responses.
The success of immediate implant placement is often challenged by the loss of bone and soft tissue, impacting the implant's initial stability. This stability is influenced by the shape of the extraction site and inflammatory infiltration, which introduces bacteria and necessitates intraoperative removal to protect healthy periodontal tissue and ensure optimal wound closure and bone healing.
Adequately addressing bone and soft tissue deficiencies around the implant is essential for the procedure's success.
The study explores a variety of bone substitute biomaterials, including autologous, allogeneic, and xenogeneic bone, bioceramics, growth factors, and natural and synthetic polymers. Autologous bone grafting, the gold standard for bone defect repair, faces limitations such as harvest site morbidity and infection risk.
Allografts and xenografts offer unlimited size and shape for defect restoration without donor site risks, though disease transmission and immune rejection are concerns. Bioceramics show promising biocompatibility and strength yet require mechanical property improvements. Growth factor materials and polymers (both natural and synthetic) exhibit excellent biocompatibility and biodegradability, with synthetic polymers providing greater toughness.
For aesthetic outcomes, the level and thickness of peri-implant soft tissues are crucial. The study reviews the use of tissue grafts and growth factor-based biomaterials for enhancing soft tissue thickness, noting the clinical preference for growth factors due to lower infection and antigenicity risks. Despite current limitations in soft tissue regeneration biomaterials, advancements in technology are expected to offer improved solutions.
Immediate implant placement is increasingly common in clinical settings, benefiting from advancements in technology and biomaterials for bone regeneration and soft tissue closure. Tissue engineering emerges as an effective strategy, offering new possibilities beyond traditional biomaterials for bone replacement. This interdisciplinary approach aims to develop implants that mimic the natural bone tissue environment, promising enhanced efficiency and outcomes in regenerative dentistry.
More information: Xiaoqi Su et al, Multiple biomaterials for immediate implant placement tissue repair: Current status and future perspectives, MedComm – Biomaterials and Applications (2024). DOI: 10.1002/mba2.69




















