This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Checking womb condition could curb cancer risk, study shows
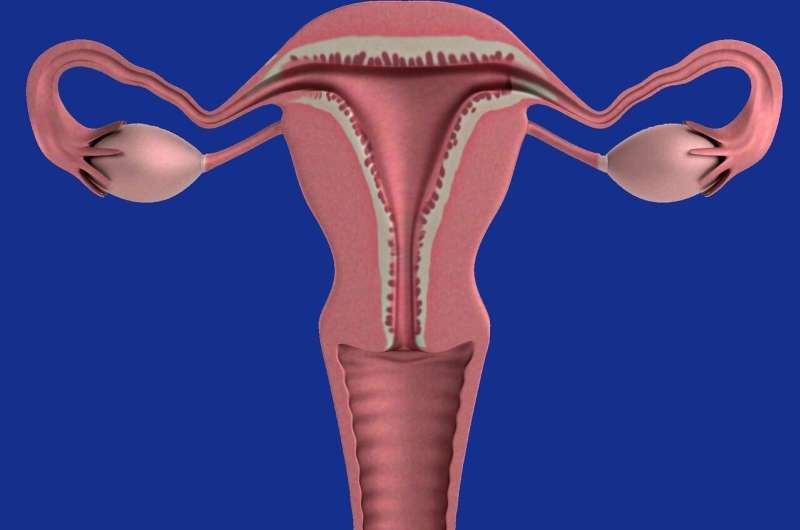
Improved patient care is needed to reduce cancer risk among women with a condition that causes excessive thickening of the womb lining, research shows.
Although treatment for those with endometrial hyperplasia has improved since national guidance was introduced in 2016, many women still do not receive adequate follow-up care.
The findings highlight the importance of ongoing work to support and manage those with the condition, experts say.
National guidance
Endometrial hyperplasia is grouped into two types—atypical and non-atypical. Atypical carries an increased cancer risk, while non-atypical indicates that the womb lining is thicker than normal but less likely to become cancerous.
UK-wide guidance for the care of those with endometrial hyperplasia recommends a hysterectomy—surgery to remove the womb—for those with the more dangerous atypical form.
Those with non-atypical endometrial hyperplasia are recommended a trial of hormone treatment given directly into the womb. Regular follow-up monitoring is vital to track potential progression to cancer.
The study, involving University of Edinburgh researchers, compared the treatment patients received before and after the introduction of national guidance. The findings have been published in PLOS Medicine.
Treatment changes
Researchers looked at anonymized patient records from more than 3,000 people across the UK diagnosed with endometrial hyperplasia between 2012 and 2020. Half had non-atypical endometrial hyperplasia and half had atypia.
The proportion of women with non-atypical endometrial hyperplasia who had successful hormone treatment increased from 38% to 52% after the guidelines were introduced.
The initial treatment of women with atypia barely changed—68% had a hysterectomy in 2012–15 and 67% in 2016–19.
This dropped to 52% of women at the start of the COVID-19 pandemic in 2020, indicating a shift away from best practice.
Monitoring recommended
Only one in five women with atypia who did not have a hysterectomy received the recommended schedule of follow-up monitoring and biopsies.
In 2016–19, 37% of those diagnosed with atypical endometrial hyperplasia who received a hysterectomy had evidence of cancer when their wombs were analyzed after surgery.
The findings emphasize the importance of improved follow-up monitoring of women with atypia who do not undergo a hysterectomy, given their high risk of co-existent cancer, experts say.
"Although there have been improvements when treating women with endometrial hyperplasia since the implementation of new national guidelines, there is a need for better care for women not undergoing a hysterectomy—particularly considering the risk of developing cancer in the future for these women," says Dr. Michael Rimmer.
More information: Ian Henderson et al, Diagnosis and management of endometrial hyperplasia: A UK national audit of adherence to national guidance 2012–2020, PLOS Medicine (2024). DOI: 10.1371/journal.pmed.1004346



















