This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study reveals dual role of protein in cancer treatment
Investigators at the UCLA Health Jonsson Comprehensive Cancer Center have uncovered new details about the role of a protein called interferon regulatory factor (IRF1) in cancer progression and treatment response, offering new insight that can potentially help improve the effectiveness of cancer immunotherapy.
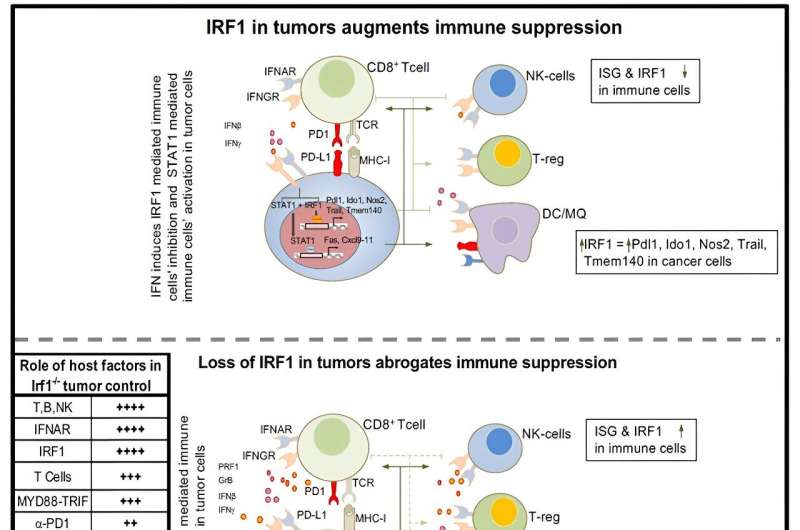
The study, published in Cell Reports, reveals how IRF1 can both hinder and help the body's immune response to tumors, depending upon which cells the protein is found in.
"We know IRF1 plays a pivotal role in modulating antiviral immunity," said Dr. Philip Scumpia, associate professor of medicine at the David Geffen School of Medicine at UCLA and senior author of the study.
"But there were conflicting reports about whether IRF1 promotes or suppresses antitumor immunity. What was surprising to us was that the role of IRF1 was different depending upon which cells expressed it, potentially explaining the conflicting reports. Our findings add a layer of complexity to our understanding of IRF1 and its role in immunotherapy."
Immunotherapy continues to be a powerful approach in cancer treatment. It works by harnessing the body's immune system to recognize and attack cancer cells. While immunotherapy has shown success in treating certain types of cancer and can lead to long-term remission in some patients, it still does not work for everyone.
Understanding the mechanisms of proteins like IRF1 can help refine immunotherapy strategies, making them more effective for a broader range of patients, noted Scumpia.
To dissect the role of IRF1 in tumor growth and immune response, the team of researchers looked at what happens when IRF1 is missing in both tumor cells and surrounding cells.
"We previously showed that cells exposed to ionizing radiation, a well-known treatment for cancer, induced an immune response through IRF1. We wanted to see whether IRF1 regulated similar immune responses in growing tumors," said Dr. Prabhat Purbey, a project scientist in the Scumpia laboratory and first author of the study.
First, the team created IRF1-deficient clones of various tumor cells and compared the growth of these genetically modified tumors to normal tumors, assessing immune cell infiltration using histology and flow cytometry. Then they examined the effect of immune checkpoint blockade therapy, a type of immunotherapy, on these tumors and performed single-cell RNA sequencing to understand the immune cell activation states.
They found that the presence of IRF1 in tumor cells can actually weaken the immune response by promoting T cell exhaustion and by affecting toll-like receptor and type-I interferon responses. This happens because IRF1 in tumor cells increases levels of several immune checkpoints, including IDO-1 and PD-L1, proteins that inhibit T cell activity while altering the expression of proteins involved in antigen presentation.
However, IRF1 is crucial for immune cell development, recruitment, and function of cytotoxic T cells and natural killer cells, key immune cells that can directly attack the tumor.
"These findings suggest that reducing IRF1 in tumor cells, or activating it in immune cells, could enhance cancer treatment effectiveness by boosting the body's natural antitumor immunity," said Scumpia, who is also a member of the UCLA Health Jonsson Comprehensive Cancer Center. "We now have a clearer picture of where IRF1 can impact immunotherapy and how we can tune it to help in the fight against cancer."
While more study is needed to understand if targeting IRF1 in tumor cells or immune cells will be beneficial after a tumor has grown in the body, this research has helped clarify why IRF1 was shown to be a hindrance or a help in different cancer scenarios.
"The potential to manipulate IRF1 in specific ways could change the way we approach cancer immunotherapy," Scumpia said. "Our goal is to translate these findings into treatments that offer real hope and improved outcomes for cancer patients."
More information: Prabhat K. Purbey et al, Opposing tumor-cell-intrinsic and -extrinsic roles of the IRF1 transcription factor in antitumor immunity, Cell Reports (2024). DOI: 10.1016/j.celrep.2024.114289



















