This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Genetically engineered dendritic cells enhance the power of immunotherapy against lung cancer
A study by researchers at the UCLA Health Jonsson Comprehensive Cancer Center suggests that injecting engineered dendritic cells directly into cancerous lung tumors can help promote a stronger immune response, causing more T cells to become active and attack the cancer more effectively.
When tested in mice with non-small cell lung cancer, the team discovered that combining this therapy with immune checkpoint blockade, a type of immunotherapy, made the treatment even more effective.
Immune checkpoint blockade has been revolutionary for treating patients with non-small cell lung cancer. However, the majority of patients with lung cancer do not benefit from the treatment and many experience disease progression after an initial response. This can occur because the immune system doesn't recognize the tumor as a threat or the environment around the tumor suppresses the immune response.
Scientists have found that certain molecules called chemokines—specifically, CXCL9 and CXCL10—play a crucial role in attracting immune cells, particularly activated T cells, to the tumor site. When these molecules are present in high amounts, they can help the immune system fight cancer more effectively.
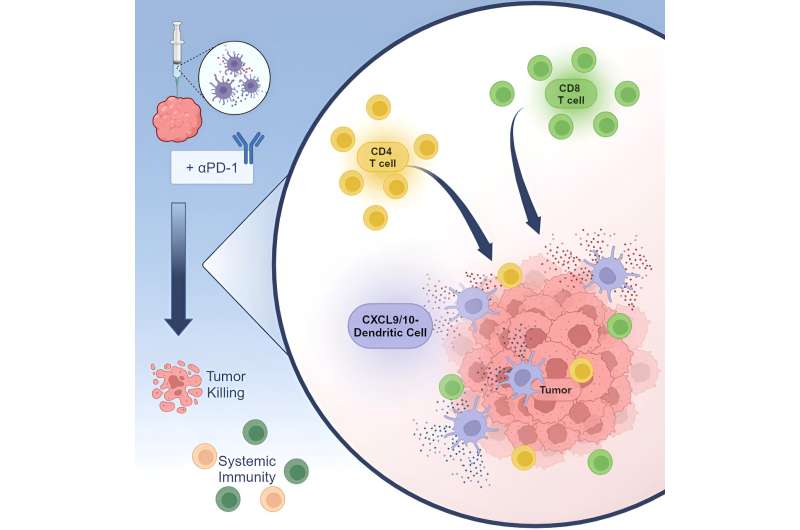
To help enhance the effectiveness of immune checkpoint blockade, the UCLA team explored an approach called in situ vaccination with gene-modified dendritic cells, which involves injecting immune-stimulating, chemokine gene-engineered dendritic cells directly into the tumor, which can boost the body's immune response against cancer.
In this study, scientists genetically modified dendritic cells to produce CXCL9 and CXCL10 to help increase T-cell infiltration and activation within the tumor. They then injected the modified dendritic cells directly into the tumors in mouse models of non-small cell lung cancer. They found that this approach increased the number and activity of T cells in the tumor and slowed down tumor growth in these models, even in cases where tumors were resistant to standard immunotherapy.
Additionally, they observed that this therapy helped to establish a long-lasting immune response against the cancer. Studies analyzing genetic data from lung cancer patients suggest that the CXCL9/10-DC therapy could be particularly beneficial for patients with certain genetic characteristics associated with resistance to standard-of-care immunotherapy.
The results of the UCLA study suggest that using CXCL9 and CXCL10-producing dendritic cells alongside immunotherapy can be a promising strategy to overcome treatment resistance and improve clinical outcomes for patients with non-small cell lung cancer.
The paper is published in the journal Cell Reports Medicine.
More information: Raymond J. Lim et al, CXCL9/10-engineered dendritic cells promote T cell activation and enhance immune checkpoint blockade for lung cancer, Cell Reports Medicine (2024). DOI: 10.1016/j.xcrm.2024.101479



















