This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study provides blueprint for hybrid-virtual home visit model to support patients who do not live close to a hospital
In a new study, a team developed and successfully tested a hybrid-virtual home visit model that provides care to veterans who do not live close to a VA health care facility. The work is published in the Journal of General Internal Medicine.
U.S. Department of Veteran Affairs (VA), Regenstrief Institute, and Indiana University School of Medicine research scientists Dawn Bravata, M.D., and Teresa Damush, Ph.D., helped lead the team.
The results from the study demonstrate the feasibility of implementing a hybrid-virtual home visit model to care for high-risk, community-dwelling older persons. Two clinical cases illustrated how this model cared for patients who might not otherwise have received timely health care.
The researchers suggest a widespread deployment of hybrid-virtual home visit model programs will be required to support the veteran population as they age in place.
"We were able to successfully convert an in-person home visit, conducted by nurse practitioners and social workers, to a hybrid-virtual model where we had a telehealth technician in the patient's home working virtually with the nurse practitioner and social worker to provide care," said Dr. Bravata, a co-principal investigator and senior author of the study.
"Having the telehealth technician drive to patients' homes allowed the nurse practitioners and social workers to telework, which gave them more time to provide patient care."
The hybrid-virtual model, known as TeleGRACE, is an extension of the established Geriatric Resources for Assessment and Care of Elders (VA-GRACE) program. VA-GRACE is a multidisciplinary care model which provides comprehensive home-based geriatric evaluation and management for older veterans residing within a 20-mile drive radius from the Indianapolis VA facility.
TeleGRACE expands access to VA-GRACE services by enrolling patients living within a 60-mile radius. TeleGRACE provides all of the same services as VA-GRACE, except it's a hybrid-virtual home visit instead of the in-person home visit. The VA has been seeking to expand access to evidence-based practices supporting community-dwelling older persons like the VA-GRACE program.
Case examples
The first case examination followed a patient scheduled for a TeleGRACE enrollment visit after being discharged from a VA in-patient admission. Before the visit, the patient sought care for a leg wound in a non-VA emergency department closer to home. Working remotely, the nurse practitioner identified that the patient needed additional follow-up care for the wound.
The nurse practitioner used pictures of the wound taken by the telehealth technician and sent them to the VA wound care service. The wound care team reviewed the pictures, determined the appropriate care, collaborated with the VA-GRACE social worker to order home-health wound care, and sent wound care supplies to the patient's home, all during the single TeleGRACE visit.
"The patient would typically have had to go through a couple of clinic visits to receive the right care if it weren't for the TeleGRACE visit. The telehealth technician provided the patient with the wound care they needed in one visit," said Dr. Bravata.
In the second case, during a TeleGRACE enrollment visit, a patient who had been discharged from a VA inpatient stay 13 days prior became unwell. The telehealth technician obtained vital signs with the nurse practitioner participating remotely.
The patient was then taken to the emergency department and admitted to the hospital for a 5-day stay. The patient told the emergency department staff and inpatient teams that the TeleGRACE program saved his life.
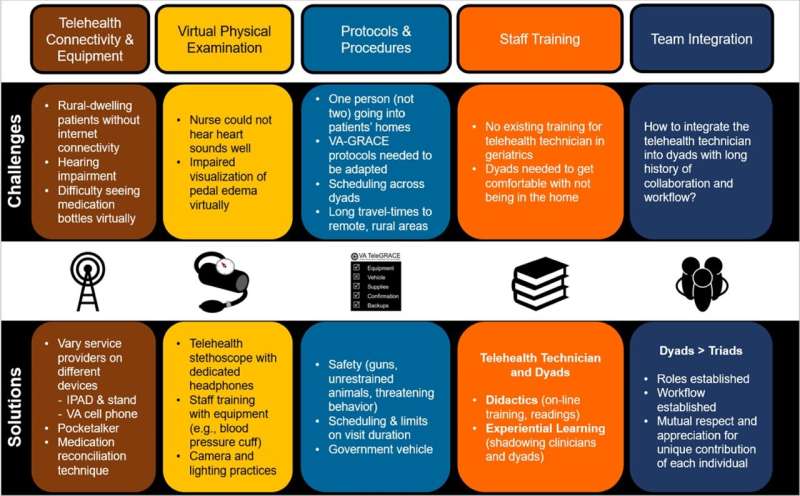
The researchers described the challenges encountered during the pre-implementation phase and the solutions they developed during program development.
"Previous studies have identified that geriatric patients have difficulty connecting with virtual health care. The TeleGRACE program overcomes many of these issues," said Dr. Bravata.
"For example, consider patients with visual or hearing impairment or perhaps mild cognitive impairment—it's helpful to have the telehealth technician physically in the homes troubleshooting equipment and providing assistance."
To implement the hybrid-virtual care model, five program domains required attention and problem-solving:
- Telehealth connectivity and equipment
- Virtual physical examination
- Protocols and procedures
- Staff training
- Team integration
More information: Cathy C. Schubert et al, Expanding Access to Comprehensive Geriatric Evaluation via Telehealth: Development of Hybrid-Virtual Home Visits, Journal of General Internal Medicine (2024). DOI: 10.1007/s11606-023-08460-5




















