This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
written by researcher(s)
proofread
Mpox is on the rise in Australia. Here's what to know about the virus—and who should get vaccinated
Australia appears to be experiencing a re-emergence of the infectious disease mpox, formerly called monkeypox.
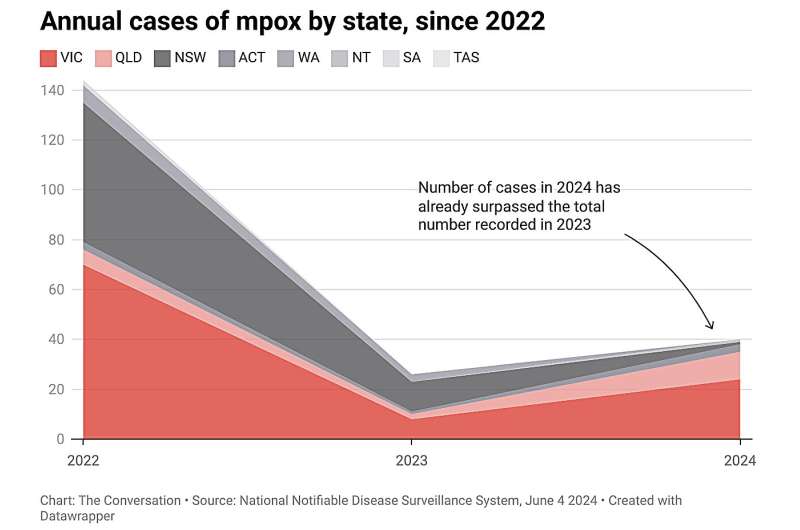
Some 40 cases have been recorded so far in 2024, already surpassing the total number recorded for 2023 (26). Victoria has reported 24 cases this year, while Queensland saw 10 cases reported in May.
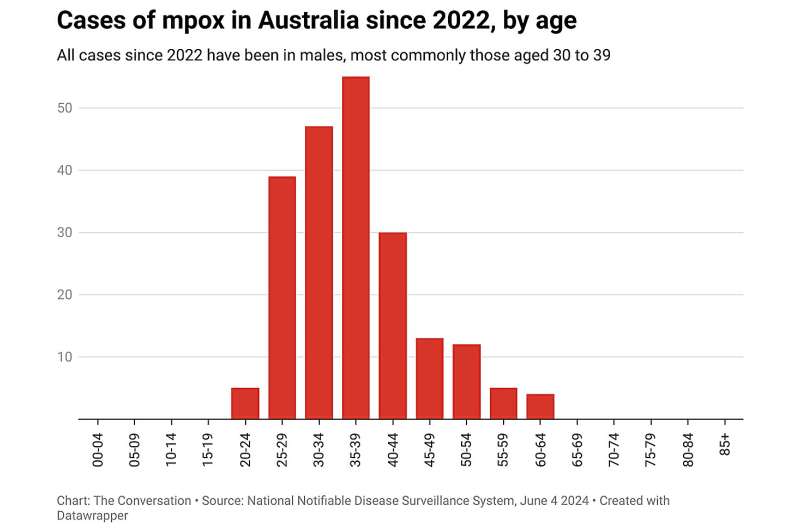
There was previously a significant mpox outbreak in 2022, with a total of 144 cases across Australia. All cases since 2022 have been in males, most commonly those aged 30 to 39. Mpox cases are on the rise elsewhere, too.
So what is mpox? And is there a vaccine available? Here's what to know about this virus.
What is mpox?
Mpox belongs to the orthopoxvirus family, which is also responsible for smallpox.
Symptoms include fever and rash, typically starting on the hands, feet and face. The genitals may also be affected. The rash is infectious until the lesions have scabbed over.
There are two clades, or varieties, of mpox: clade I and clade II. Up to 10% of people infected with clade I may die, compared to 1% or less of those infected with clade II.
Traditionally, both clades of mpox have been endemic in countries in central and western Africa, where it transmits from animals to humans, and has occasionally caused human outbreaks.
Mpox outbreaks began occurring outside Africa in 2018, with cases detected in the United Kingdom, Israel and Singapore in people traveling from Nigeria, which began experiencing outbreaks in 2017.
The 2022 epidemic spread to non-endemic regions such as Europe, the Americas, and Australia, with more than 97,000 cases confirmed globally to date.
These outbreaks were caused by clade IIb, a variant of clade II, with case fatality below 1%. Clade IIb is also behind the current cases in Australia.
How does mpox spread?
Recent research indicates both clades of mpox are undergoing rapid mutations, with genetic changes in clade I that may enhance its transmissibility among humans.
These mutations suggest a shift from its historical zoonotic transmission patterns toward sustained human-to-human spread.
Mpox spreads between people primarily through close contact with infected lesions or bodily fluids. Sexual transmission accounts for most of clade IIb's spread, especially among high-risk groups like gay, bisexual, and other men who have sex with men.
The pattern of spread appears different for the two clades. Like smallpox, mpox is a respiratory virus and has been found in ambient air, so respiratory transmission is possible.
Clade I is causing large epidemics in the Democratic Republic of Congo (DRC), with more than 20,000 suspected cases since 2023.
The estimated fatality rate in DRC is 4.6%, with 70% of cases and close to 90% of deaths in children under 15.
This suggests respiratory and close-contact transmission are the primary modes of spread in DRC. However, sexual transmission of clade I has also been reported.
Vaccination is our best bet
The primary strategy for preventing further outbreaks of mpox in Australia is vaccination. The recommended shot is the JYNNEOS vaccine, which was developed as a smallpox vaccine.
Older smallpox vaccines are made from a live virus called vaccinia, a related orthopoxvirus that protects against smallpox and mpox. The older vaccines have fully replicating vaccinia virus in them, which can be risky for people with weakened immune systems. The JYNNEOS vaccine is modified so the vaccinia virus doesn't replicate in the body and is safer for people with conditions such as HIV.
For full protection, two doses are required at least 28 days apart. Two doses given before exposure to the virus is 84% effective in preventing mpox and protection is believed to last for at least a couple of years.
Cases may still occur in people who are vaccinated, but these infections are typically milder.
The vaccine is also effective after exposure to the virus, but less so than if it's given beforehand.
Who should get vaccinated?
Australian guidelines recommend vaccination in gay, bisexual, and other men who have sex with men. They also recommend vaccination for sex workers, and people with HIV who may be at risk of exposure to mpox.
Health-care workers who treat or are likely to treat patients with mpox are advised to consider having the vaccine.
Post-exposure vaccination is recommended for people who public health authorities classify as having had a high-risk mpox contact in the previous 14 days.
Australia's approach to the 2022 mpox outbreak involved ensuring early access to vaccination and working closely with LGBTQ+ community and health organizations. These organizations raised awareness of mpox symptoms, modes of transmission, and vaccination.
In 2023, 48% of gay and bisexual men in Sydney and Melbourne reported having received at least one dose of mpox vaccine. Rapid uptake of vaccines may have contributed to low rates of mpox in Australia.
Future focus
It appears mpox has become established as a sexually transmitted infection in gay, bisexual, and other men who have sex with men. Achieving and maintaining high rates of vaccination in this group will be crucial in long-term prevention efforts.
Ongoing surveillance is also important, while contact tracing will help minimize the size of any clusters, facilitating post-exposure vaccination where warranted. In Australia, state and territory health departments have extensive experience in contact tracing and work with affected communities.
Australia has so far been successful in avoiding a major epidemic, including in early 2023 when Sydney WorldPride brought thousands of gay men from around the world to Sydney.
In the next few years, unequal access to vaccination around the world will likely mean continued introductions of mpox from settings with lower vaccination rates. Ensuring equitable vaccine access is vital to global and local disease control.
A global approach to controlling mpox is essential, as infections in one country can spread rapidly internationally, as the 2022 epidemic showed.
This article is republished from The Conversation under a Creative Commons license. Read the original article.![]()



















