This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Societal and biological factors both contribute to mental health issues in the wake of COVID-19
Even as classrooms, offices, concerts and weddings have begun to look more like their pre-2020 counterparts, marks of the global pandemic remain visible in new norms and long-term issues.
"COVID-19 affected a whole generation of individuals at every level," said Khalid Afzal, MD, a pediatric psychiatrist at the University of Chicago Medicine.
In conversations on social media and in other forums, many people share a general sense that COVID-19 had a significant impact on mental health—that it represents a collective trauma from which we will be healing for years. Now that researchers have a few years' worth of data to analyze, they're beginning to unpack that mental impact more fully from an empirical standpoint.
The toll of upheaval
According to Afzal, attempted suicide and suicide-related emergency department visits for both children and adults went up significantly within a few months of the pandemic's onset, as did completed suicide rates. Data from the CDC and researchers across the country also show a jump in rates of disorders like anxiety and depression, and psychiatric treatment centers have reported longer wait times as demand exceeded capacity.
"After a few months, the reality hit people that the situation wasn't going to change anytime soon," Afzal said. "And the more they became isolated, the more that isolation compounded with other stressors like financial worries and fear of dying. It's pretty disheartening to see the toll it took on people."
He said the interruption of major life milestones like graduations was especially traumatizing for children and adolescents, as were the lack of privacy and relational tensions caused by families being cooped up in close quarters.
How a respiratory virus can affect the brain
It makes sense that the pandemic's massive societal disruptions triggered mental distress. Less obvious—but still important—are the direct impacts of biological changes from COVID-19 that affect the brain and behavior.
Although COVID-19 is first and foremost a respiratory virus, it attacks many systems in the body and can cause dangerous inflammation. Health experts quickly realized that adults with particularly serious psychiatric disorders, such as schizophrenia and bipolar disorder, were uniquely vulnerable to COVID-19 infection—their cases were more likely to be medically severe, and many experienced worsening of their psychiatric disorders. "It wasn't necessarily an intuitive outcome, but the trend became clear very early on," said Royce Lee, MD, a psychiatrist and researcher at UChicago Medicine.
People who didn't have psychiatric diagnoses before contracting COVID-19 weren't invulnerable to neurological effects, either. Many wound up with "long COVID" symptoms like pain, mental cloudiness, lack of sustained attention, difficulty with memory, depression, anxiety, fatigue and irritability.
"There are causal pathways in both directions between immune activation and brain function, which affect behavior and emotions," said Lee, whose research often focuses on those pathways. "In particular, there's a very strong connection between immune activation and regulating anger." Immune activation can come directly from the virus itself or be triggered indirectly by stress and fear.
Lee pointed out that even people who don't notice brain fog or have detectable "long COVID" may still experience subtler symptoms like increased irritability, so it's important to continue the destigmatization of mental health and encourage awareness to help people take back control of their emotions.
"If abrupt shifts in mental health show up, it's still relevant to ask yourself, 'When was my last COVID-19 infection? And how does the timing of that align with my change in mental state?'" Lee said.
Staying proactive about mental health and safety
Elevated rates of suicide and psychiatric disorders make mental health safety an especially high priority in the wake of COVID-19. A group of UChicago researchers recently published a study highlighting safety concerns related to a substance found in countless homes: acetaminophen.
"It's important to think about how something that's so easily accessible could be used for something very dangerous," said first author Wendy Luo, a third-year student at the UChicago Pritzker School of Medicine. "As the pandemic unfolded and kids started to struggle even more with mental health, it makes sense that they've often turned to what's available in the home."
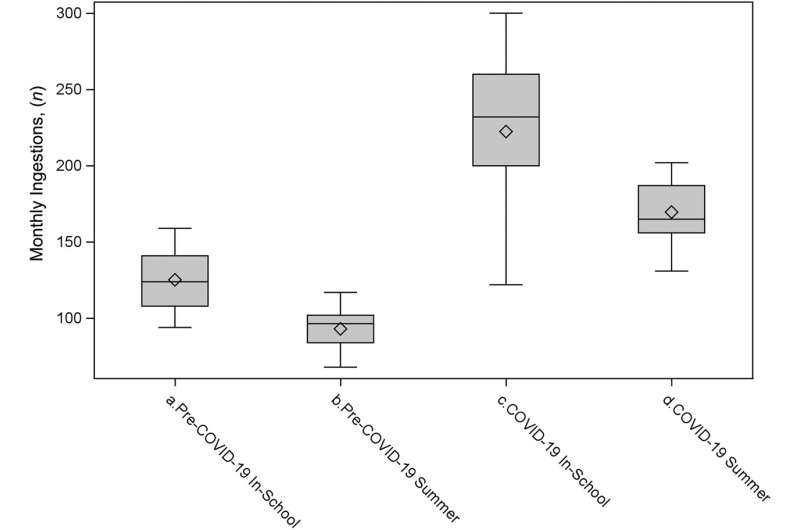
Even before 2020, researchers had noticed an increase in calls to poison control hotlines related to suspected attempted suicide by acetaminophen overdose. Experts also documented higher suicide rates among students during the academic year compared to the summer months. Luo and her collaborators set out to investigate whether COVID-19 exacerbated these trends even further.
They compared acetaminophen-related hospital admissions from the pre-COVID-19 era (January 2016–February 2020) to the COVID-19 era (March 2020-December 2022). They found that intentional acetaminophen ingestion became much more frequent during the COVID-19 era among children ages 8-18, and the rates remained highest during the school year even though many schools were at least partially remote during that time period.
"We're hoping these results send a message that we need to have more resources in schools because we consistently see the highest rates of self-harm during the months students spend in school," Luo said. "And when there are major disruptions in school like the shift from in-person to virtual and hybrid during the pandemic, some children struggle even more with the uncertainty and isolation."
Moving forward as COVID-19 lingers
"As a society, we need to educate ourselves, recognize that these mental effects are very real, and provide individualized support and accommodations for people as they recover," Afzal said. "It's important to view people as survivors rather than victims. I think people are naturally resilient, but the way we talk about things affects the way we move forward."
Like Luo, Afzal pointed out the need for more resources in multiple settings. He said some hopeful trends have already emerged, such as an increase in the number of medical students choosing to specialize in psychiatry, but added that there is plenty of room for various decision-makers to increase mental health care capacity and provide a wider range of solutions and support.
Lee likes to refer back to the Spanish flu as a good teaching case for understanding some of the effects of a worldwide pandemic. Fortunately, the past may have some hope to offer:
"There was kind of a delayed response: in the two or three years following that viral outbreak, psychiatric disorders increased in prevalence and some new ones emerged, probably as a result of immune activation," he said. "It was almost like a neuropsychiatric second wave of the pandemic. But then it got quiet again and more or less went back to normal. I think it's possible we'll see similar trends with this pandemic."
"COVID-19 and Intentional Toxic Pediatric Acetaminophen Ingestions: A Research Brief" was published in Hospital Pediatrics in April 2024. Authors included Wendy Luo, Isabella Zaniletti, Sana J. Said and Jason M. Kane.
More information: Wendy Luo et al, COVID-19 and Intentional Toxic Pediatric Acetaminophen Ingestions: A Research Brief, Hospital Pediatrics (2024). DOI: 10.1542/hpeds.2023-007424




















