This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Study finds health care providers would recommend human papillomavirus self-collection
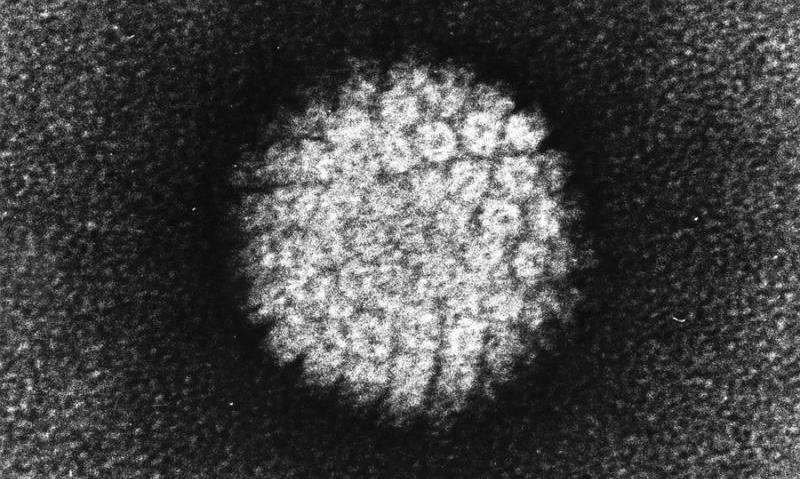
In 2019, more than 12,000 new cases of cervical cancer were diagnosed and upwards of 4,000 patients died in the U.S. The causal link between human papillomavirus (HPV) infection and the development of cervical cancer is well documented. Cervical cancer screening guidelines are currently in the review process for updates.
On May 15, 2024, the U.S. Food and Drug Administration (FDA) approved patient-collected testing (vaginal self-collection) for HPV. Several countries, including the Netherlands and Australia, have introduced HPV self-collection as a part of their national screening programs.
In a new study from Boston University Chobanian & Avedisian School of Medicine and the University of Hawaii at Manoa School of Nursing, researchers found more than half of health care providers would definitely or possibly offer HPV self-collection to their patients if the FDA approved the procedure, indicating substantial acceptance of this technology among the health care provider community.
The findings are published in the journal Women's Health Issues.
"Health care providers felt that self-collection would be particularly beneficial for those who did not have access to clinician-collected screening, as well as for patients who may have difficulty with pelvic exams for any reason, such as those with history of trauma, sexual or gender minority patients and those with mobility issues," explained senior author Rebecca B. Perkins, MD, MSc, professor of obstetrics & gynecology at BU and an obstetrician & gynecologist at Boston Medical Center.
This study incorporated a mixed methods design including conducting a national survey and interviews of health care providers who perform cervical cancer screening. Quantitative measures consisted of provider/practice characteristics, willingness to recommend and preferences related to self-collection. Interviews further elucidated the provider perspectives.
The study found that male providers, advanced practice providers, internal and family physicians, and those practicing in an academic medical center, hospital, or community health setting were more likely to support self-collection than female participants, OB-GYN physicians, and those in private practice.
"While we found providers considered HPV self-collection to be a way to expand access for patients, they also expressed concerns related to the quality of the sample in generating accurate results," added Holly Fontenot, Ph.D., RN/NP, FAAN, professor of nursing at University of Hawaii and lead author of the study.
According to the researchers, the recent approval of HPV self-collection in the U.S. provides another option for cervical cancer screening, which can help reduce barriers related to access or to personal medical conditions.
More information: Holly B. Fontenot et al, Health Care Provider Willingness to Recommend Self-collected Tests for Human Papillomavirus: A Mixed Methods Examination of Associated Factors, Women's Health Issues (2024). DOI: 10.1016/j.whi.2024.05.005




















