This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Prenatal Zika infection in mothers found to have long-term immune consequences in children, even without microcephaly
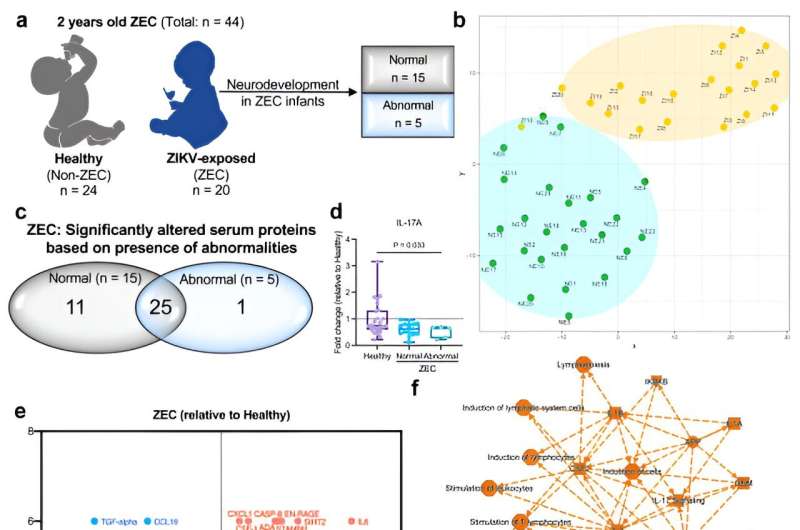
A Cleveland Clinic-led study published in eBioMedicine reveals that maternal Zika virus infections can reprogram fetal immune development, leading to long-term consequences for children's immunity. These changes even occur in children born without the physical characteristics associated with congenital Zika syndrome—suggesting that the 95% of babies born of Zika-infected pregnancies who did not exhibit symptoms may have been affected by the virus with long-term immunological repercussions.
Only 5% of children whose mothers experienced Zika infections during pregnancy are born with physical or neurological disabilities and diagnosed with congenital Zika syndrome. Suan-Sin (Jolin) Foo, Ph.D., a world-renowned expert in maternal-fetal virology and the Zika virus, says babies without these symptoms are deemed healthy and do not receive any follow-up medical care or attention.
"Studies have only really focused on what's happening with the children who were born with visible physical conditions like microcephaly or neurological complications," she says. "The rest of these kids may not even have a note on their chart mentioning that their mother was infected during pregnancy. Unless they're part of our study, they're essentially lost to the medical field."
Dr. Foo, Weiqiang (Javier) Chen, Ph.D., and Jae Jung, Ph.D., director of Cleveland Clinic's Sheikha Fatima bint Mubarak Global Center for Pathogen & Human Health Research, teamed up for an international study that began with a large Zika virus outbreak in Brazil in 2015. The Cleveland Clinic team collaborated with clinician researchers Karin Nielsen-Saines, MD, University of California, Los Angeles, and Patricia Brasil, MD, Ph.D., and Fundação Oswaldo Cruz (Fiocruz) in Rio de Janeiro, Brazil who run a large clinical cohort studying the effects of Zika virus infection on fetal development in Rio de Janeiro.
The study used blood samples from newborn and two-year-old children whose mothers were infected by Zika virus during pregnancy. Immune analysis revealed highly elevated levels of inflammation, even two years after the Zika virus infection was cleared. The affected children's immune systems also favored producing one type of T-cell over another, altering their responses to childhood vaccines. These changes left them likely vulnerable to future infections including diphtheria, tetanus and pertussis.
Immune problems were not correlated with any other physical or neurological symptoms of congenital Zika syndrome, including microcephaly or neurodevelopmental delays. The presence of long-term immunological alterations in children who were deemed unaffected by Zika at birth shows an entire group of pregnancy-related Zika complications that fell through the cracks, Dr. Foo says.
Dr. Foo's lab is now conducting studies to understand how the Zika virus causes these changes in fetal immune development, with the goal of developing treatments to block or reverse the virus's effects. They are also hopeful that their findings will challenge the current understanding of how Zika virus affects pregnancy and encourage more researchers and funding agencies to study long-term effects of prenatal Zika infection.
"The medical field has a very specific definition of congenital Zika syndrome. The children must have impaired skull or brain development," says Dr. Foo. "Our study clearly shows that there's much more to this condition than meets the eye. We need to expand diagnostic criteria and conduct more research to make sure these immunologically vulnerable children get the care they need."
More information: Suan-Sin Foo et al, Sustained chronic inflammation and altered childhood vaccine responses in children exposed to Zika virus, eBioMedicine (2024). DOI: 10.1016/j.ebiom.2024.105249




















