Breakdown of bone keeps blood sugar in check, new study finds
Researchers led by Columbia University Medical Center have discovered that the skeleton plays an important role in regulating blood sugar and have further illuminated how bone controls this process. The finding, published in Cell, is important because it may lead to more targeted drugs for type 2 diabetes.
Led by Gerard Karsenty, MD, PhD, chair of the Department of Genetics and Development at Columbia University Medical Center, the researchers found that the destruction of old bone during normal skeletal regrowth - a process known as resorption - is necessary to maintain a healthy level of glucose in the blood.
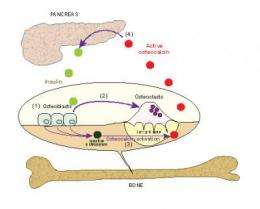
While resorption is a process that occurs throughout life to make way for new bone, Dr. Karsenty's team discovered that it also acts to stimulate the release of insulin into the bloodstream and improve the uptake of glucose by cells in the entire body.
The findings suggest that, for some people, diabetes may develop from changes in the skeleton, and that drugs designed to stimulate the bone-insulin pathway may lead to better drugs for type 2 diabetes.
The first clue that the skeleton may have an important role in regulating blood glucose came in 2007 when Dr. Karsenty discovered that a hormone released by bone - known as osteocalcin - can regulate glucose levels. Osteocalcin turns on the production of insulin in the pancreas and improves the ability of other cells to take in glucose. Both of these processes are impaired in type 2 diabetes.
The new paper reveals that osteocalcin cannot work until cells that degrade bone start working and begin the resorption process. As the cells degrade bone, inactive osteocalcin is converted to its active form by the increase in acidity around the bone.
"Remarkably, insulin was discovered to favor bone resorption. Hence, in a feed-forward loop it favors the activation of osteocalcin, which in turn favors insulin synthesis and secretion," said Dr. Karsenty. "Insulin is a street-smart molecule that takes advantage of the functional interplay between bone resorption and osteocalcin, to turn-on the secretion and synthesis of more insulin."
By identifying the tight connection existing between energy metabolism and skeleton physiology - in this case between insulin and osteocalcin - this new study further underscores the wealth of physiological function exerted by the skeleton. The finding further strengthens the idea that diabetes could be treated by increasing the level of osteocalcin in the body. In addition, the researchers suggested that since most drugs to treat another condition - osteoporosis - work by inhibiting bone resorption, the drugs may decrease the activation of osteocalcin and cause glucose intolerance in some patients.
"This research has important implications for both diabetes and osteoporosis patients," said Dr. Karsenty. "First, this research shows that osteocalcin is involved in diabetes onset; secondly, bone may become a new target in the treatment of type 2 diabetes, the most frequent form of diabetes, as it appears to contribute strongly to glucose intolerance; and, finally, osteocalcin could become a treatment for type 2 diabetes."
"And for people with osteoporosis, the concern is that a common treatment, bisphosphonates - which work by inhibiting bone resorption and therefore may increase glucose intolerance, could push someone with borderline glucose intolerance into full-fledged disease onset. Although, more research is needed to study this further," said Dr. Karsenty.
















