Medication used to control blood sugar in people with type 2 diabetes may also reduce risk of autoimmune diseases
Dipeptidyl peptidase-4 inhibitors commonly used to control blood sugar levels in people with type 2 diabetes may also reduce the risk of autoimmune diseases in these patients, according to research presented this week at the American College of Rheumatology Annual Meeting in San Diego.
Dipeptidyl peptidase-4 inhibitors (commonly called DPP-4 inhibitors) such as linagliptin (Tradjenta), saxagliptin (Onglza), and sitagliptin (Januvia) are approved by the United States Food and Drug Administration for the treatment of type 2 diabetes. Researchers recently studied how often people with type 2 diabetes taking a DPP-4 inhibitor developed autoimmune diseases—such as rheumatoid arthritis, lupus, inflammatory bowel disease, psoriasis and multiple sclerosis—when compared to those not taking one.
"DPP-4 is a transmembrane glycoprotein widely expressed in various cells and is also involved in the immune system," says Seoyoung C. Kim, MD, MSCE; assistant professor of medicine; Division of Pharmacoepidemiology & Pharmacoeconomics; Division of Rheumatology, Immunology and Allergy at Brigham and Women's Hospital in Boston and lead investigator in the study. "Prior studies suggested a potential role of DPP4i as a novel therapy for several inflammatory diseases by inhibiting T-cell proliferation and cytokine production. Our hypothesis was that patients with type 2 diabetes starting a DPP4i would have a reduced risk of incident RA and other autoimmune diseases compared to those patients starting non-DPP4i hypoglycemic agents."
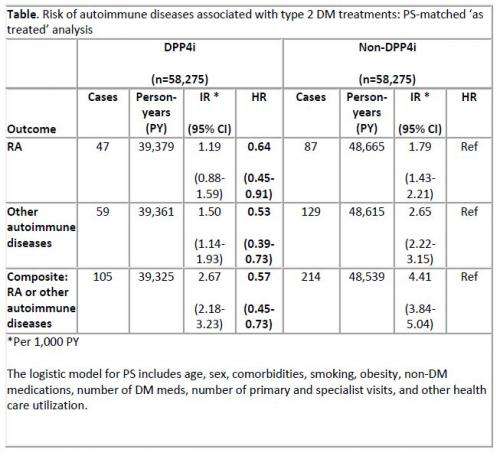
Using the data from United States commercial insurance claims from 2005 to 2011, Dr. Kim's team compared two mutually exclusive groups: 58,275 patients with type 2 diabetes starting DPP4i combination therapy with patients with type 2 diabetes starting non-DPP4i combination therapy.
Patients taking insulin, or with pre-existing systemic autoimmune diseases, HIV or cancer were excluded.
Rheumatoid arthritis and other autoimmune diseases were defined with two or more diagnosis codes that were seven or more days apart and one or more prescriptions for disease-specific immunosuppressive drugs or steroids. Potential confounders such as age, sex, co-existing conditions, diabetes-related factors, medications, and health care utilization were controlled for in the analysis.
Dr. Kim's team found that patients with type 2 diabetes who were starting a DPP-4 inhibitor appear to be at a lower risk of developing RA or other autoimmune diseases compared to those starting non-DPP4i drugs. Although the overall incidence rate of RA or other autoimmune diseases was low (approximately one in 1,000), patients taking DPP4i combination therapy appeared to be 34 percent less likely to develop RA and 27 percent less likely to develop the other autoimmune diseases. Subgroup analysis comparing DPP4i to sulfonylurea showed similarly protective effect of DPP4i on autoimmune diseases, but not comparing DPP4i versus thiazolidinediones.
"Among patients with type 2 diabetes, initiating DPP4i combination therapy may be associated with a decreased risk of rheumatoid arthritis or other autoimmune diseases compared to initiating non-DPP4i combination therapy," explains Dr. Kim. "Although our results are not definitive, these results may contribute to the understanding of new mechanistic pathways for preventing or delaying the onset of autoimmune diseases. It could also lead to a potential new therapeutic approach. Future research is needed to determine the effect and safety of DPP4i in the non-diabetic population."
Patients should talk to their rheumatologists to determine their best course of treatment.
More information: Kim, S. et al. Dipeptidyl Peptidase-4 Inhibitors In Type 2 Diabetes May Reduce The Risk Of Autoimmune Diseases
















