B-cells aggravate autoimmune diseases
Scientists in Freiburg may have discovered a fundamental aggravating factor in autoimmune diseases. If B-lymphocytes lack the protein PTP1B, the cells will become hyperactive for stimulatory signals and can thus promote an autoimmune attack. This study offers an additional explanation to how B-cells regulate an immune response.
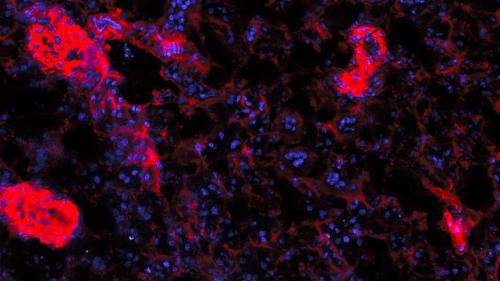
In Germany, approximately 800,000 people suffer from rheumatoid arthritis. In this progressive disease, a person's own immune system attacks and destroys connective tissue. However, the most important factors governing the progress of the disease are still unknown. Now, scientists working with Michael Reth and David Medgyesi from the Max Planck Institute of Immunobiology and Epigenetics have identified a factor that may play a significant role. Using genetic engineering, they deactivated the PTP1B protein in B-cells in the immune systems of mice. The B-cells then became much more responsive to activating signals and, in turn, served to reactivate the other cells.
PTP1B could therefore have a monitoring function in the B-cell-mediated immune response. Until now, B-cells were mainly known for producing antibodies after coming into contact with pathogens. Only recently is more and more accepted by researchers that B-lymphocytes possess important regulatory function in the immune system. The current study now provides a new detail of this mechanism.
A clinical investigation showed that B-cells in patients suffering from rheumatoid arthritis also produce unusually low amounts of the studied protein. In the patients' other cell types, and in healthy subjects, this was not the case. "This suggests that the protein plays a significant role in the development or the aggravated course of rheumatoid arthritis", says principal investigator Michael Reth. Reth is head of the Molecular Immunology department at the Max Planck Institute of Immunobiology and Epigenetics, as well as scientific director of the Centre for Biological Signalling Studies (BIOSS), a German Cluster of Excellence at the University of Freiburg.
In cases of rheumatoid arthritis in which conventional treatments are ineffective, patients can be treated with the drug Rituximab. The drug destroys all B-cells in the body and will thus at least halt the progress of the disease. "The B-cells produced after the Rituximab therapy possess similar amount of the PTP1B protein as cells in healthy people. This may contribute to the less severe autoimmune reaction", explains first author David Medgyesi. Long-term studies are required to determine whether these newly produced cells will lose the protein over time.
By the end of the 1990s, the laboratory headed by Michael Reth had already developed mice with B-cells in which specific genes could be knocked out using Cre-lox technology. In the meantime, this mouse strain is being used very successfully in over 200 laboratories around the world to study the functioning of the immune system.
More information: Medgyesi D, Hobeika E, Biesen R, Kollert F, Taddeo A, Voll RE, Hiepe F, and Reth M. The protein tyrosine phosphatase PTP1B is a negative regulator of CD40 and BAFF-R signaling and controls B cell autoimmunity. Journal of Experimental Medicine, DOI: 10.1084/jem.20131196










