Smarter, cheaper technologies offer improved point-of-care medicine
Scientists have developed and combined new paper and flexible polymer substrates with special sensing devices for rapid and accurate detection of pathogens such as HIV, as well as other biotargets. These novel technologies offer the type of robust, simple, and inexpensive biosensing systems required to provide point-of-care health care in remote areas, where there is minimal diagnostic infrastructure or equipment and a lack of trained medical technicians.
A team from Stanford University School of Medicine (Bio-Acoustic MEMS in Medicine Labs) developed assays for the simple and rapid detection of HIV-1, various bacteria, and CD4+ T lymphocytes. The assays for pathogens and cells were used as proof of concept to demonstrate the utility of several new detection and sensing technologies.
Overall, the group has developed platforms and sensing devices that are easy to make, easy to use and can be safely disposed of after use—characteristics necessary for developing affordable tools with broad applications in both developed and developing countries. The work is reported in the March 6 edition of Nature Scientific Reports.
"The group is simultaneously developing multiple novel methods that target important diseases in underserved communities," says Tiffani Lash, PhD., Director of the NIBIB Program in Point-of-care Technologies. "Their comprehensive approach is resulting in smarter, inexpensive technologies that can be applied to a wide range of health care problems and settings."
Testing for HIV-1 in whole blood
Current tests for HIV infection detect antibodies to HIV in the individual's blood. However, because it takes up to several months for those antibodies to form, these tests do not detect individuals in the earliest stage of infection when they are most likely to pass on the disease. In order to detect HIV-1 in recently infected individuals the researchers developed an assay that can detect the presence of the virus in whole blood or plasma.
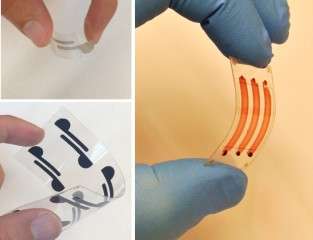
The platform is a disposable flexible polyester chip with implanted electrodes. HIV-1 antibodies are added to whole blood or plasma where they bind to the virus creating aggregates of antibody and viral lysate. When added to the flexible chip, the aggregates change the electrical conductivity of the chip, which gives a simple electrical readout indicating that the sample contains HIV-1. In addition to detecting early stage infection, the electrical readout is much simpler and less expensive than current assays. The researchers estimate that the cost is about $2 per test and can be safely disposed of after use.
CD4+ T Lymphocyte capture and detection
Accurate CD4+ T cell count is essential for HIV-1 diagnosis and treatment monitoring. World Health Organization guidelines recommend antiretroviral therapy for individuals with a CD4+ T cell count of less than 500 cells/ml. Conventional CD4+ T cell counting methods require an expensive flow cytometer, a skilled operator, and costly reagents. A disposable and flexible biosensing platform for efficient counting of CD4+ T cells has potential to address some of these global health challenges in the point-of-care setting.
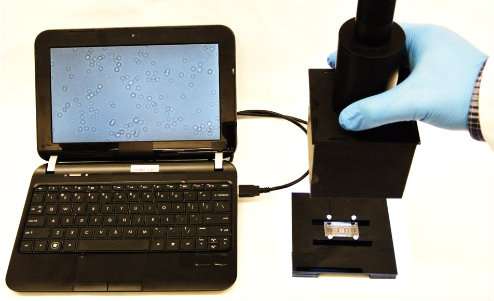
The approach used by the research team to develop a simple, inexpensive assay for CD4+ T cell count involved two novel technologies: a polyester film with microfluidic channels to capture the T cells, and a detection technology known as lensless shadow imaging. The microfluidic channels were coated with an antibody that captures the CD4+ T cells. A single drop of whole blood from a fingerprick was applied to the polyester film, where capillary forces pull the blood into the microfluidic channels. The shadow of the CD4+ T cells that adhere to the channels can then be visualized on the polyester film.
Overall, the platform allows efficient CD4+ T cell counting using fingerprick volume of unprocessed whole blood samples on disposable film at the point-of-care. This platform has the potential to replace the current use of non-disposable glass platforms that require additional steps and expense to visualize the cells with a fluorescent tag.
Using a cell phone to detect and quantify bacteria
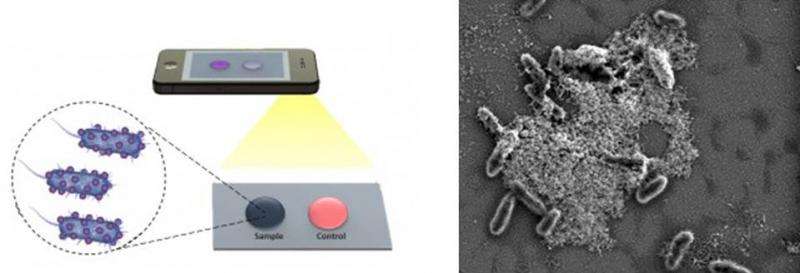
E. coli and S. aureus are the most common bacterial pathogens that cause food poisoning, skin infections and blood infections. The group developed a sensitive biosensing platform that detects E. coli by the aggregation of nanoparticles on cellulose paper.
Gold nanoparticles are covered with surface molecules that bind to E. coli bacteria. When the test fluid containing bacteria is mixed with the nanoparticles and transferred to the cellulose paper, the aggregation results in a blue spot. If bacteria are not present, there is no aggregation and the solution applied to the cellulose paper turns red. Thus the presence or absence of bacteria can be seen immediately. Further, the group was able to determine the concentration of E.coli in the sample by taking a picture of the blue spot on the paper with a cell phone and using an imaging analysis tool to measure red pixel intensity of the picture. Concentrations of E. coli could be quantified ranging from 8 to 1.5 million bacteria per milliliter. Further, the platform provides a multiplexed capability and can be applied to other bacteria such as S. aureus.
"The goal of our work," says Utkan Demirici, PhD., of the Demirici Bio-Acoustic-MEMS in Medicine Laboratory at Stanford School of Medicine, "is to simplify the techniques that both capture the biotarget and detect that captured target. Both aspects of a simplified test must be addressed to move this type of work forward to practical use in low resource settings. These platform technologies can be potentially broadly applied to other diseases such detecting oncogenic viruses such as KSHV, HPV, HBV and HCV, which we also need to be monitored in the developed world settings at a primary care physicians office or during a dental appointment or at the bedside. "
More information: Paper and flexible substrates as materials for biosensing platforms to detect multiple biotargets. Shafiee H, Asghar W, Inci F, Yuksekkaya M, Jahangir M, Zhang MH, Durmus NG, Gurkan UA, Kuritzkes DR, Demirci U. Sci Rep. 2015 Mar 6;5:8719. DOI: 10.1038/srep08719



















