How are cancer patients diagnosed? And could it be better?

Around 330,000 people are diagnosed with cancer in the UK every year, and each of them will have a different story to tell.
Some will be diagnosed after seeing their GP. For others, it will be after a visit to hospital. And some will be diagnosed via one of the UK's screening programmes.
Among these is a category of diagnosis that we know has the lowest survival – people diagnosed in an emergency. This might be via a hospital's Accident & Emergency (A&E) department, or after their GP spots symptoms that need to be looked into immediately. In other cases, a hospital doctor may spot something alarming while a patient's already being treated for something else.
But how many patients are diagnosed in each of these different ways? And can we find ways to reduce the number of emergency diagnoses?
In 2010, the National Cancer Intelligence Network (NCIN) – an organisation that analyses data on cancer patients in England – began to answer these questions, by analysing healthcare data and patient records in its first 'Routes to Diagnosis' report.
It found that around one in four cancer patients is diagnosed in an emergency, suggesting that there was great potential for improvement.
Next week, then NCIN will publish an updated report. In preparation for the new data, we thought we'd take an in-depth look at the different ways (or 'routes') patients are diagnosed, particularly at what we mean by an 'emergency' – and at how understanding and collecting this information can help improve cancer care.
Many roads to travel
There are many different ways cancer can be diagnosed, but the NCIN classifies them into seven main groups:
- Screening – people diagnosed via the National Screening Programmes for bowel, breast and cervical cancers.
- Urgent GP referrals for suspected cancer ('Two-week wait') – people diagnosed after their GP, concerned that their symptoms could be caused by cancer (e.g. unexplained jaundice in an older person), quickly referred them for further tests that should take place within two weeks.
- Routine GP referral – people who see a GP due to unexplained symptoms which don't initially arouse a suspicion of cancer, but which need investigating, e.g. someone with persistent raised lymph glands but no other symptoms.
- During a hospital appointment ('Other outpatient') – this refers to people who need to visit hospital for monitoring or tests, and their doctors spot a cancer, e.g. someone being monitored for a liver disease known as 'fatty liver', whose scans show liver cancer.
- Whilst admitted to hospital ('Inpatient elective') – people whose cancer is picked up while staying in hospital for treatment or monitoring. For example, if someone is in hospital for pneumonia and a lung tumour is spotted on an X-ray.
- Emergencies – As we'll see below, this complex category is when cancer is picked up after a patient is seen in an 'emergency' – we'll discuss what this means in more detail below
- Unknown – This is due to incomplete data, for example when all that a patient's records show is that they had cancer treatment on the NHS. Many patients diagnosed privately are in this group, because private healthcare providers aren't required to record data in the same way as the NHS.
The graphic below shows the proportion of patients are diagnosed via these different routes, based on the NCIN's 2010 analysis (we'll update this when the new data's released next week).
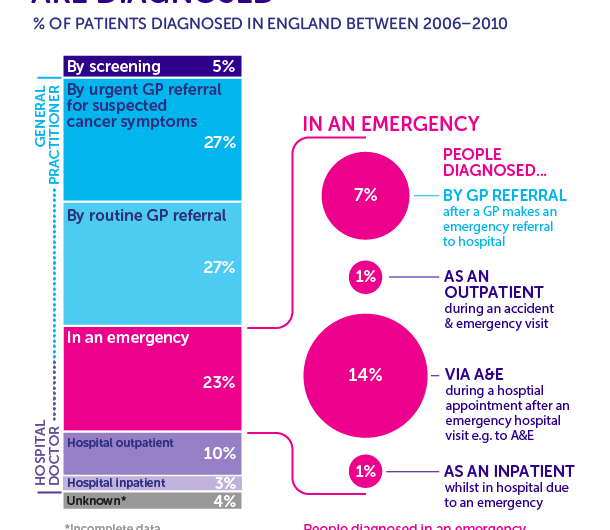
The NCIN's initial findings were stark: one in four patients (23 per cent) diagnosed between 2006 and 2010 were diagnosed in an emergency, making it the second most common way people were diagnosed.
As we've said above, this matters. These patients tend to have worse outcomes, either because their cancer is more aggressive, or because it's more advanced. And this latter point suggests that at least some of these people would have benefited from earlier diagnosis.
But what do 'emergencies' actually mean? And what can we do about them?
Many different types of emergency
The word 'emergency' might evoke images of flashing blue lights and BBC1's 'Casualty', but the reality is more complex, reflecting the fact that cancers can be hard to diagnose.
And while the majority diagnosed in an emergency are diagnosed after going A&E, emergency diagnoses also include patients that first saw doctors in other parts of the NHS. About a third of these people visited their GP with symptoms that meant they needed an immediate, emergency transfer to hospital.
Much smaller numbers of people were admitted straight to hospital in an emergency (inpatients). That includes situations such as elderly people being transferred from a nursing home to hospital in an emergency, and then being diagnosed with cancer.
There are also some people that go to A&E or are admitted to hospital in an emergency, but are discharged and then diagnosed in a subsequent follow-up appointment at the hospital (outpatients).
And to add to that complexity, some of these emergencies won't necessarily be caused by cancer. There are many non-cancer emergencies – such as car accidents and heart attacks – that require specialist care and diagnostics, that can lead to a cancer being diagnosed incidentally (something clinicians call an 'incidentaloma').
Because of these many different types of emergency, it means there isn't a single solution to improve things. But understanding them does mean we can begin to ask more intelligent questions in the search for answers.
Different cancers develop symptoms differently
We can find out more by looking at how emergency rates vary according to the type of cancer a patient has. Different cancer types develop differently, have different symptoms, and pose different challenges to doctors and patients. And this ultimately means that some cancers are much more likely to be diagnosed in an emergency than others.
Consider brain tumours and acute leukaemias. Over six out of 10 (63 per cent) patients with brain tumour or with a type of leukaemia called acute lymphoblastic leukaemia, are diagnosed as emergencies. This emphasises what doctors tell us about these cancers – they often cause vague symptoms, or symptoms that only appear once the disease is already fairly advanced.
Where the tumour is located in the body also affects when certain symptoms appear, particularly if it's an organ deep within the body, such as the lungs or pancreas.
So when symptoms appear late or are vague sometimes, emergencies can be unavoidable. And given that there aren't reliable diagnostic tests that can routinely detect these cancers early, these can even be considered the best medical care that person could receive: doctors are doing their very best to spot these cancers in time to give patients treatment.
But among these emergencies, we know that there are people who do show symptoms at an early stage, but who aren't diagnosed early.
How can we help both the general public, and GPs, spot those cancers and avoid an emergency later on?
Spotting vague cancer symptoms
The answer is complex, but has two key themes – public awareness, and GP support.
There's evidence that patients who have potential cancer symptoms, but who dismiss their symptoms as trivial, or who worry about wasting the doctor's time, may decide against going to their GP. It also appears that older people, and people from more socio-economically deprived areas, are less likely to seek help.
And that's where public awareness campaigns such as Be Clear on Cancer in England and Detect Cancer Early in Scotland can help. These campaigns encourage people to see their GP if they notice anything unusual or persistent, and while it's not yet clear if they can reduce emergency diagnoses they had promising results.
But GPs also have a difficult challenge in spotting cancers with vague symptoms, and there's also work going on to try to improve things here.
Each GP practice carries out regular Significant Event Analysis (SEA), to review how they handled patients who turned out to have serious diseases like cancer. This allows them to identify cases where they felt there was room for improvement, so that they can try to find opportunities to do better in the future.
One thing that's begun to emerge from SEAs is that it's important for GPs to make follow-up appointments with patients with certain symptoms, to see if they persist – a practise called 'safety-netting'.
GPs should also be helped by new guidelines, published earlier this year, that give them more flexibility to refer patients with suspected cancer symptoms.
But that will only make a difference if the government and NHS ensure there's enough investment in diagnostic services (something were we're campaigning for via our Test Cancer Sooner campaign).
Are things improving?
Since 2010, there's been a lot of change in the health service – some positive, some not so positive.
As the new figures will only go up to 2013, we won't be able to look at the impact of substantial the NHS reforms that came in that year. So what are we expecting to see next week when the new data are published?
On the plus side, there have been big improvements in the way the NHS collects data, which should make the upcoming results a more accurate reflection of cancer care in England.
We've also seen awareness campaigns, such as Be Clear on Cancer, which we hope will have helped encourage people to see their GP earlier. And there has been a huge amount of work to find ways to diagnose cancer earlier, as exemplified by the National Awareness and Early Diagnosis Initiative, which we're proud to be leading.
So overall, we're optimistic – we're expecting to see fewer people diagnosed in an emergency, more diagnosed by GPs via the 'two-week wait', and we're hoping to pick up more clues to keep focusing efforts to ensure this trend continues. We'll be posting an update next week when the new data are published. Stay tuned.
More information: "The role of primary care in cancer diagnosis via emergency presentation: qualitative synthesis of significant event reports." British Journal of Cancer (2015) 112, S50–S56. DOI: 10.1038/bjc.2015.42



















