Discovery could lead to a new animal model for hepatitis C
During its career, the potentially fatal hepatitis C virus has banked its success on a rather unusual strategy: its limitations. Its inability to infect animals other than humans and chimpanzees has severely hampered scientists in developing a useful small animal model for the disease. But now, in a breakthrough to be published in the January 29 advance online issue of Nature, Rockefeller University scientists have identified a protein that allows the virus to enter mouse cells, a finding that represents the clearest path yet for developing a much-needed vaccine as well as tailored treatments for the 170 million people across the globe living with the tenacious, insidious and rapidly changing virus.
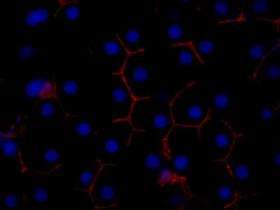
By using a genetic screen, the group, led by Charles M. Rice, head of the Laboratory of Virology and Infectious Disease, identified a human protein, called occludin, that makes mouse cells susceptible to the virus. The discovery means that scientists now have the complete list of cellular factors — a total of four — that are required for the virus to enter nonhuman cells.
The hepatitis C virus exclusively targets human liver cells, suggesting that these cells express genes that allow uptake of the virus, genes that are not expressed in other human and nonhuman cells, explains Rice. In past years, three proteins — CD81, CLDN1 and SR-BI — were identified as having key roles in shuttling the virus into cells, but something was clearly missing. Rice's group found that even when they engineered mouse cells to overexpress all three proteins, the cells still denied the virus entry.
The discovery of occludin, however, has changed that. When Rice and his colleagues engineered mouse and human cell lines to express all four proteins, they showed that each cell line became infectible with the virus. To further establish occludin's role as a required entry factor, the group showed that human liver cells naturally express high levels of occludin, and that by silencing its expression, they could give these once highly susceptible liver cells the ability to completely block infection.
"You know, you sort of have to get lucky," says Rice, who is also Maurice R. and Corinne P. Greenberg Professor at Rockefeller. "You've got these three factors you know are important, but you could have 10 other human factors that could have been necessary for hepatitis C virus entry. This work shows that's not the case."
In their DNA screen, the team, including Alexander Ploss, a research associate in the lab, and Matthew J. Evans, currently at Mount Sinai School of Medicine in New York, first cloned all the genes that were expressed in liver cells and then delivered them to mouse cells. "Then, going through an iterative screening process, we honed in on the genes that made the mouse cells permissive," says Ploss, who spearheaded the project with Evans.
Since mice and humans each have a species-specific version of the four factors, the group used hamster cells to see which combination of factors did the best job at making the cells infectible. They found that in the case of two of the proteins, occludin and CD81, only the human versions worked; for SR-BI and CLDN1, the human and mouse versions did an equally good job. These experiments not only suggest that there may be more than one potential animal model, but also that there are several specific combinations of entry factors that could generate them.
"This work provides a clear foundation upon which we can now begin to construct an animal model for the uniquely human pathogen," says Rice. "This is only a first step but in terms of creating an animal model for hepatitis C, it's a big leap forward."
Source: Rockefeller University



















