Cellular Source of Most Common Type of Abnormal Heart Beat Found
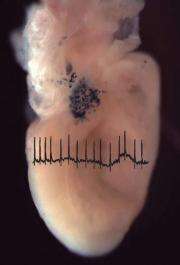
(PhysOrg.com) -- While studying how the heart is formed, scientists at the University of Pennsylvania School of Medicine serendipitously found a novel cellular source of atrial fibrillation (AF), the most common type of abnormal heart beat.
Jonathan Epstein, MD, William Wikoff Smith Professor, and Chair, Department of Cell and Developmental Biology, and Vickas Patel, MD, PhD, Assistant Professor of Medicine, have identified a population of cells in the atria of the heart and pulmonary veins of humans and mice that appear to be the seat of AF. The finding may lead to a more precise way to treat AF, with reduced side effects. Their findings appear online in the Journal of Clinical Investigation.
This group of cells expresses the protein DCT, which is also involved in making the skin pigment melanin and in the detoxification of free radicals. The researchers also showed that the DCT-expressing cells in the mouse heart were a distinct cell type from heart-muscle cells and pigment-producing cells, although they conduct electrical currents important for coordinated contraction of the heart. The location of these cells in the pulmonary veins suggested their possible role in AF because AF can arise in these blood vessels. Atrial fibrillation is a very common and debilitating disease that greatly affects quality of life.
Know ing the location of these cells may help develop better treatments for AF. "We already target the pulmonary veins for radiofrequency ablation, a nonsurgical procedure using radiofrequency energy similar to microwaves, to treat some types of rapid heart beating as a relatively new treatment, and sometimes cure, for AF," notes Epstein.
"For the most part, current drug therapy for atrial fibrillation has been disappointingly ineffective and drug therapy is often associated with burdensome side-effects," notes Patel."
"If these cells are truly the source of AF in some patients, and we can figure out a way to identify them, then our ablation can be far more precise and targeted, thus limiting potential side effects, making the procedure potentially more simple and rapid, and hence more cost effective," explains Epstein.
But the investigators caution more research is needed to get to the point where these ideas can be validated in patients. "The findings hold out promise for a more precise cellular target for treating this common disorder," adds Epstein.
Provided by University of Pennsylvania School of Medicine (news : web)















