A lab rat -- created in the lab
It's illegal for health products with medical formulations to be accepted by the U.S. Food and Drug Administration without tests on animals -- a situation that has serious ethical and moral implications. New research in the field of tissue engineering by Prof. Amit Gefen of Tel Aviv University's Faculty of Engineering holds a promise that far fewer lab animals will be needed for the necessary experimental trials.
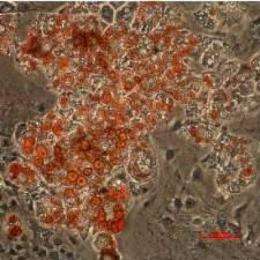
Dr. Gefen's research into fat cells, published in a recent issue of Tissue Engineering, has led him to conclude that the necessary tissue can be produced from fat, skin, bone and muscle cells. His breakthrough study could have hundreds of applications in the pharmaceutical and medical world.
"Drugs make our lives better, and basic science is needed to push new drugs through clinical trials. But there is no doubt that an untold number of animals are sacrificed in the laboratory setting -- both in basic research and in applied conditions when testing particular molecules," says Prof. Gefen, who heads TAU's Teaching Laboratory for Cell and Tissue Engineering. As a medical researcher himself, he was dependent on animal trials for testing new hypotheses he developed for living systems ― until recently.
A more efficient road to scientific research
Bridging the worlds of biology and engineering, Prof. Gefen is now using adult rat stem cells ― cells that can be stimulated to create skin, bone, fat and muscle tissue from an animal in a laboratory setting. In his own work on studying the mechanical properties of pressure ulcers, many tissue replications were needed. His new approach no longer requires the sacrifice of large numbers of animals. When an experiment is over, not one animal life has been lost.
The use of engineered tissues, says Prof. Gefen, may also be more scientifically efficient than using those from a living source. "The model we've created offers a very reliable method for researchers asking questions about basic science, and those investigating new drugs. We can injure tissue in a very controlled environment and grow muscle tissue without blood vessels, thereby neutralizing certain variables that often cloud what's happening in an experiment."
Saving lives and improving research at the same time
Though Prof. Gefen's method may not completely eliminate the need for animal testing, as few as 5% of the animals used today will need to be sacrificed in future tests, he predicts.
"It's a matter of proportion. Our tools spare an enormous number of lives," Prof. Gefen says. He is currently bringing together a number of discrete research directions from the separate fields of mechanics, tissue engineering and biology. He is also developing a new tool for researchers to investigate fat accumulation in cells (an important question for diabetes researchers) and weight loss drugs. Among his devices is one that can tell doctors how much mechanical stress is being placed on a person's foot, buttocks or other soft tissues. Another measures how much sensation is left in a diabetic limb. For all these approaches, Prof. Gefen has adopted tissue engineering methods to use fewer animals in his trials.
"We are now able to build a number of 'simplified' living tissues quite readily, and we're able to keep them 'alive,'" Prof. Gefen says. "They're genetically similar to the biological tissue of the animal, so we can factor out irrelevant physiological elements such as bleeding and pain response in an experiment. The fact that this tissue is genetically identical and the environmental factors are so well-controlled means that we can obtain far more experimental reproducibility than with experiments done on live animals."
In the future, Prof. Gefen hopes that similar models can be based on live human tissue, but that could be a number of years down the road.

















