October 27, 2011 report
Neuroimmunologists find gut bacteria link to multiple sclerosis
(Medical Xpress) -- Researchers at the Max Planck Institute of Neurobiology have found that commensal gut flora in mice is an essential part of the immune triggering process that leads to multiple sclerosis (MS). In their paper published in Nature, the team led by Gurumoorthy Krishnamoorthy and Hartmut Wekerle write that microbial environmental factors that lead to the disease aren’t able to do their work in the absence of common gut bacteria, thus they find that such bacteria are a necessary link in the chain of events that lead to the broad spectrum neurological disease known as MS.
People get MS when the myelin sheaths that cover the axons of the brain and spinal cord begin to deteriorate due to attacks by the immune system. This results in nerve cells that are unable to communicate with one another leaving those affected with an individualized set of symptoms ranging from numbness, tingling and muscle loss to problems in hearing, vision and swallowing. And while the particular environmental microbial factors that start the process are still unknown, this new research by the team in Germany shows that the process can’t continue without assistance from at least some of the bacteria that exist in the gut.
The researchers discovered the gut bacterial link by subjecting test mice that had been genetically engineered to develop MS like symptoms, to doses of antibiotics to kill off all of their gut bacteria. As a result they found that the immune system in the mice no longer attacked the myelin sheaths, thus they never got MS. When gut bacteria were then subsequently introduced however, eighty percent of the mice then developed symptoms.
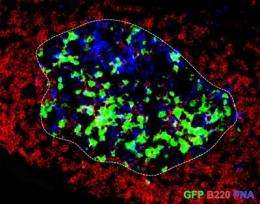
Despite this new lead, scientists are still stymied as to what sort of genetic disposition leads the immune system in some people to react to certain unknown microbial factors which appears to lead to excited T cells winding up in the lymph nodes and comingling with B cells, which then together travel to the brain and spinal cord where they begin to attack the myelin coating on the nerves they find there.
The next step in the research project will be a process of elimination to try to figure out which gut bacteria in particular are necessary for the chain of events to proceed.
More information: Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination, Nature (2011) doi:10.1038/nature10554
Abstract
Active multiple sclerosis lesions show inflammatory changes suggestive of a combined attack by autoreactive T and B lymphocytes against brain white matter. These pathogenic immune cells derive from progenitors that are normal, innocuous components of the healthy immune repertoire but become autoaggressive upon pathological activation. The stimuli triggering this autoimmune conversion have been commonly attributed to environmental factors, in particular microbial infection. However, using the relapsing–remitting mouse model of spontaneously developing experimental autoimmune encephalomyelitis, here we show that the commensal gut flora—in the absence of pathogenic agents—is essential in triggering immune processes, leading to a relapsing–remitting autoimmune disease driven by myelin-specific CD4+ T cells. We show further that recruitment and activation of autoantibody-producing B cells from the endogenous immune repertoire depends on availability of the target autoantigen, myelin oligodendrocyte glycoprotein (MOG), and commensal microbiota. Our observations identify a sequence of events triggering organ-specific autoimmune disease and these processes may offer novel therapeutic targets.
© 2011 PhysOrg.com















