Fighting melanoma's attraction to the brain
(Medical Xpress)—The process of metastasis, by which cancer cells travel from a tumor site and proliferate at other sites in the body, is a serious threat to cancer patients. According to the National Cancer Institute, most recurrences of cancer are metastases rather than "new" cancers.
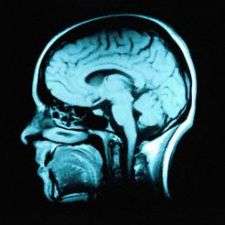
Virtually all types of cancer can spread to other parts of the body, including the brain. Once metastatic melanoma cells are entrenched in the brain, patients typically have only a few months to live.
Now Prof. Isaac Witz and his team at Tel Aviv University's Department of Cell Research and Immunology are delving deeper into what attracts metastatic melanoma cells to the brain, and how they survive and prosper in this environment. Their experiments have discovered that melanoma cells produce receptors for two chemokines—a family of small proteins secreted by cells—present in the brain tissue. These receptors may act as a homing device, drawing the cancerous cells to the brain.
"These interactions between the chemokines in the brain and the melanoma cell receptors could be potential targets for new therapies," Prof. Witz says. "With medications that suppress these molecules, you could hope to interfere with this specific migration." Published in the International Journal of Cancer, this research is supported by the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation.
A dangerous attraction
Although metastasis is a well-understood process, researchers are still trying to uncover the underlying mechanisms of why cancer cells begin to migrate in the first place. It is also crucial to understand what allows them to sustain themselves, divide, and propagate once they have arrived at their new location.
To better understand metastacized melanoma cells in the brain, the researchers cultured brain tissue in the lab, then analyzed all of the materials that were expressed by the cells. They identified certain chemokine receptors in brain-metastasizing melanoma cells and corresponding chemokines in the brain tissue which could ultimately be responsible for the cancer cells' being "attracted" to the brain. If a certain chemokine is released from the brain, and the melanoma cells have the appropriate receptors, a chemical attraction will take place where the melanoma cells would be drawn to wherever the chemokine is.
Duplicating nature
The researchers have also developed a method to compare metastatic and non-metastatic cells with identical genetic backgrounds. Though they are derived from the same cancer, some of these cells become metastatic, while others do not. "This is a good way for us to concentrate on the genes that are specific to metastatic cells. Because we have these two types of cellular variants, where only one goes to the brain and metastasizes, it's an important tool" for future research, explains Prof. Witz.
The researchers have found that mice that are inoculated with non-metastatic cells do end up with melanoma cells in the brain, but they are dormant and do not generate overt metastasis. The key is to discover why these originally identical cells differ—why the non-metastatic cells don't develop in the same way.
Understanding the process will help scientists to "duplicate what nature does, and prevent these cells from becoming metastatic," says Prof. Witz. "If there already is metastasis, it is too late—so what we want to do is to prevent development by understanding the mechanism that keeps the non-metastatic cells dormant."













