Lack of iron regulating protein contributes to high blood pressure of the lungs
A protein known to regulate iron levels in the body has an unexpectedly important role in preventing a form of high blood pressure that affects the lungs, and in stabilizing the concentration of red cells in blood, according to a study in mice by researchers at the National Institutes of Health.
In mice, lack of iron regulatory protein 1 (Irp1) results in pulmonary hypertension, a form of high blood pressure that affects the lungs, and to polycythemia, a rare disorder in which the body produces excess red blood cells.
"This insight might lead to progress in treating cases of polycythemia or pulmonary hypertension without a known cause," said senior author Tracey A. Rouault, M.D., of the Division of Intramural Research (DIR) at the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), where the research was conducted. It's possible, she added, that human cases of these disorders might result from malfunctioning copies of the gene for Irp1.
The study also provides insight into how the body directs iron into the manufacture of blood to prevent anemia, the deficiency of red blood cells.
The findings appear in Cell Metabolism.
Dr. Rouault collaborated with more than a dozen other NIH researchers, including first authors Manik C. Ghosh, Ph.D., and Deliang Zhang, Ph.D., also of the NICHD's DIR, as well as researchers at the NIH Veterinary Resources Program and the National Heart, Lung and Blood Institute. Researchers from the University of Colorado School of Medicine, Denver, and the University of Nebraska–Lincoln were also part of the team.
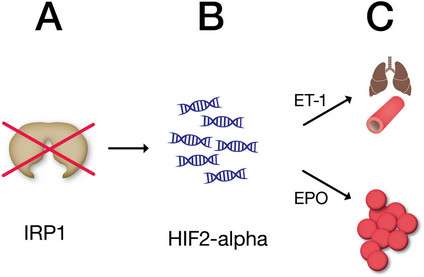
Iron regulatory protein 1 (Irp1) detects iron levels in cells and directs either the storage or use of iron, depending on other conditions in the body. The researchers found that mice lacking Irp1 produced high levels of hypoxia inducible factor 2-alpha (HIF2 alpha), a protein produced in response to low oxygen conditions, like those that occur at high altitudes. In turn, HIF2 alpha spurs production of the hormone erythropoietin, which stimulates the production of red blood cells.
When the animals were put on low-iron diets, they did not become anemic, but instead developed polycythemia and pulmonary hypertension.
In people, polycythemia and high blood pressure in the lungs are rare conditions, and in some cases occur without a known cause. It is possible that changes in the gene for Irp1 may account for some of these cases, the researchers suggest.
To investigate Irp1's role in regulating the body's use of iron, the researchers reared mice lacking the gene that makes Irp1 and divided the animals into two groups, feeding one group a normal diet and the other a low iron diet.
Within a year, less than 40 percent of the mice on the low-iron diet had survived. Most had died from abdominal hemorrhaging. The researchers found that the mice on low iron diets had high levels of HIF2 alpha in the lungs and kidney. These animals produced high levels of erythropoietin, which resulted in polycythemia. HIF2 alpha also triggered increased production of a substance known as endothelin-1 in the lungs, which likely contributed to the development of pulmonary hypertension.
"Irp1 appears to be the switch that controls whether HIF2 alpha protein is made," Dr. Zhang said.
This research also provided insight into how Irp1 functions under normal circumstances Dr. Rouault explained. The researchers theorize that in low-iron conditions, Irp1 allows the production of HIF2 alpha. HIF2 alpha then triggers production of erythropoietin, to generate more red blood cells. To supply iron for the red blood cells, iron is removed from the tissues. When tissue iron levels decline too much, Irp1 halts production of HIF2 alpha, and production of new blood cells ceases, conserving the body's remaining iron stores. Production of red blood cells then declines, leading to anemia.
















