Fibromyalgia is not all in your head, new research confirms
Fibromyalgia, a painful condition affecting approximately 10 million people in the U.S., is not imaginary after all, as some doctors have believed. A discovery, published this month in Pain Medicine/i> (the journal of the American Academy of Pain Medicine), clearly now demonstrates that fibromyalgia may have a rational biological basis located in the skin.
Fibromyalgia is a severely debilitating affliction characterized by widespread deep tissue pain, tenderness in the hands and feet, fatigue, sleep disorders, and cognitive decline. However, routine testing has been largely unable to detect a biological basis for fibromyalgia, and standard diagnosis is based upon subjective patient pain ratings, further raising questions about the true nature of the disease. For many years, the disorder was believed to be psychosomatic ("in the head") and often attributed to patients' imagination or even faking illness. Currently approved therapeutics that provide at least partial relief to some fibromyalgia patients are thought to act solely within the brain where imaging techniques have detected hyperactivity of unknown origin referred to as "central sensitization." However, an underlying cause has not been determined, leaving many physicians still in doubt about the true origins or even the existence of the disorder.
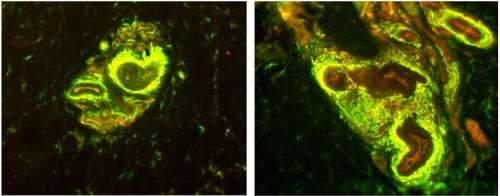
Now, a breakthrough discovery by scientists at Integrated Tissue Dynamics LLC (Intidyn), as part of a fibromyalgia study based at Albany Medical College, has provided a biological rationale for this enigmatic disease. The small biotechnology research company, founded by neuroscientists Dr. Frank L. Rice and Dr. Phillip J. Albrecht, reports on a unique peripheral neurovascular pathology consistently present in the skin of female fibromyalgia patients which may be a driving source of the reported symptoms.
"Instead of being in the brain, the pathology consists of excessive sensory nerve fibers around specialized blood vessel structures located in the palms of the hands," said Dr. Rice, President of Intidyn and the senior researcher on the study.
"This discovery provides concrete evidence of a fibromyalgia-specific pathology which can now be used for diagnosing the disease, and as a novel starting point for developing more effective therapeutics."
Nerve Endings Come In Many Forms
Three years ago, Intidyn scientists published the discovery of an unknown nervous system function among the blood vessels in the skin in the journal PAIN.
As Dr. Rice explained, "we analyzed the skin of a particularly interesting patient who lacked all the numerous varieties of sensory nerve endings in the skin that supposedly accounted for our highly sensitive and richly nuanced sense of touch. Interestingly however, this patient had surprisingly normal function in day to day tasks. But, the only sensory endings we detected in his skin were those around the blood vessels". Dr. Rice continued, "We previously thought that these nerve endings were only involved in regulating blood flow at a subconscious level, yet here we had evidencs that the blood vessel endings could also contribute to our conscious sense of touch… and also pain."
Now, in collaboration with renowned Albany Medical Center neurologist and pain specialist Dr. Charles E. Argoff, the study primary investigator, and his collaborators Dr. James Wymer also at Albany Medical College and Dr. James Storey of Upstate Clinical Research Associates in Albany, NY, clinical research proposals were funded by Forest Laboratories and Eli Lilly. Both pharmaceutical companies have developed FDA-approved medications with similar functions (Serotonin/Norepinephrine Reuptake Inhibitors, SNRI) that provide at least some degree of relief for many fibromyalgia patients.
"Knowing how these drugs were supposed to work on molecules in the brain," Dr. Albrecht added, "we had evidence that similar molecules were involved in the function of nerve endings on the blood vessels. Therefore, we hypothesized that fibromyalgia might involve a pathology in that location". As the results demonstrate, they were correct.
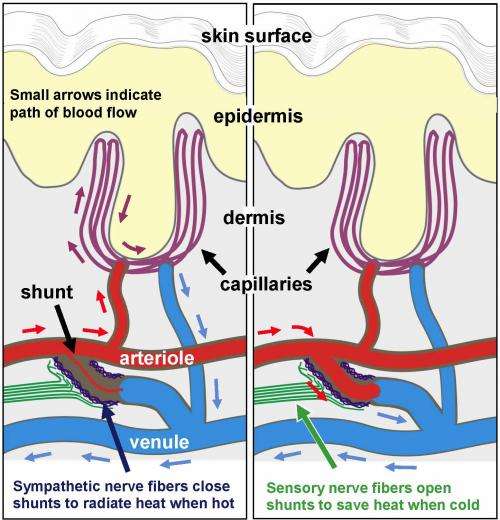
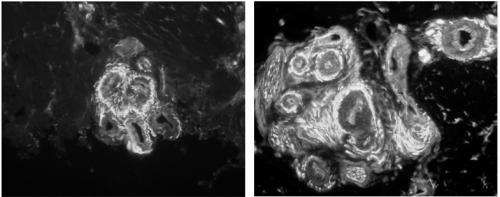
To analyze the nerve endings, Drs. Rice, Albrecht, and postdoctoral researcher Dr. Quanzhi Hou, used their unique microscopic technology to study small skin biopsies (less than half the size of a pencil eraser) collected from the palms of fibromyalgia patients, who were being diagnosed and treated by Drs. Argoff, Wymer, and Storey. The study was limited to women, who have over twice the occurrence of fibromyalgia than men. What the team uncovered was an enormous increase in sensory nerve fibers at specific sites within the blood vessels of the skin. These critical sites are tiny muscular valves, called arteriole-venule (AV) shunts, which form a direct connection between arterioles and venules (see diagram).
As Dr. Rice describes their function, "We are all taught that oxygenated blood flows from arterioles to capillaries, which then convey the deoxygenated blood to the venules. The AV shunts in the hand are unique in that they create a bypass of the capillary bed for the major purpose of regulating body temperature."
A Thermostat for the Skin
In humans, these types of shunts are unique to the palms of our hands and soles of our feet which work like the radiator in a car. Under warm conditions, the shunts close down to force blood into the capillaries at the surface of the skin in order to radiate heat from the body, and our hands get sweaty. Under cold conditions, the shunts open wide allowing blood to bypass the capillaries in order to conserve heat, and our hands get cold and put on gloves.
According to Dr. Albrecht, "the excess sensory innervation may itself explain why fibromyalgia patients typically have especially tender and painful hands. But, in addition, since the sensory fibers are responsible for opening the shunts, they would become particularly active under cold conditions, which are generally very bothersome to fibromyalgia patients."
A role in regulating blood flow throughout the body.
Although they are mostly limited to the hands and feet, the shunts likely have another important function which could account for the widespread deep pain, achiness, and fatigue that occurs in fibromyalgia patients. "In addition to involvement in temperature regulation, an enormous proportion of our blood flow normally goes to our hands and feet. Far more than is needed for their metabolism" noted Dr. Rice. "As such, the hands and the feet act as a reservoir from which blood flow can be diverted to other tissues of the body, such as muscles when we begin to exercise. Therefore, the pathology discovered among these shunts in the hands could be interfering with blood flow to the muscles throughout the body. This mismanaged blood flow could be the source of muscular pain and achiness, and the sense of fatigue which are thought to be due to a build-up of lactic acid and low levels of inflammation fibromyalgia patients. This, in turn, could contribute to the hyperactvity in the brain."
Dr. Albrecht also points out that alterations of normal blood flow may underlie other fibromyalgia symptoms, such as non-restful sleep or cognitive dysfunctions. "The data do appear to fit with other published evidence demonstrating blood flow alterations to higher brain centers and the cerebral cortex of fibromyalgia patients" he stated. Senior Research Chair of the Alan Edwards Center for Pain Research at McGill University, Dr. Gary Bennett, commented after seeing the results that "It is exciting that something has finally been found. We can hope that this new finding will lead to new treatments for fibromyalgia patients who now receive little or no relief from any medicine."
This discovery of a distinct tissue pathology demonstrates that fibromyalgia is not "all in your head", which should provide an enormous relief to fibromyalgia patients, while changing the clinical opinion of the disease and guiding future approaches for successful treatments.
More information: Albrecht PJ, Hou Q, Argoff CE, Storey JR, Wymer JP, Rice FL (2013). Excessive Peptidergic Sensory Innervation of Cutaneous Arteriole-Venule Shunts (AVS) in the Palmar Glabrous Skin of Fibromyalgia Patients: Implications for Widespread Deep Tissue Pain and Fatigue. Pain Medicine, May 20. doi: 10.1111/pme.12139 [Epub ahead of print]. www.ncbi.nlm.nih.gov/pubmed/23691965















