Antibiotics are good, right? Well think again
The University of Sydney is building relationships with medical researchers at major universities in Chile, Argentina and Brazil. Jon Iredell, who recently visited Latin America to meet research partners, talks to Richard North about the potentially fatal infections that take healthy people off the street and put them into intensive care.
In affluent, First World Australia, infectious diseases such as encephalitis, severe respiratory infections and septic shock are low on our list of medical anxieties. As Jon Iredell puts it, the general feeling is that we don't get into trouble from infections. Cancer and obesity are our problems.
But the perception that medical science has already won the fight against infections is contradicted by the statistics. "If you look at the raw data from Australia, you can see what the killers are," says Professor Iredell, Director of the NHMRC Centre for Research Excellence in Critical Infection at the Sydney Medical School.
"We all know about road trauma, but three times as many people die from overwhelming infection, or septic shock."
Septic shock causes more deaths overall than breast or bowel cancer. It is a true medical emergency, and in around one in three cases, the patient will die in hospital. Doctors must choose effective antibiotics immediately and without the aid of diagnostic tests. At present it takes a day or more to identify the antibiotic susceptibility of the causative bacteria - but every hour's delay in providing effective antibiotic therapy increases the risk of dying significantly.
"In some parts of the world, 50 or 60 per cent of serious bacterial infections are antibiotic-resistant," says Professor Iredell. In Australia only 5 to 10 per cent are resistant to common hospital antibiotics, although this figure is rising. So, in an emergency like septic shock, powerful broad-spectrum antibiotics still work very well here."
Unfortunately, antibiotics also indiscriminately kill bacteria that that we rely on to keep us healthy. Professor Iredell explains: "Transient extinctions of bacterial populations may be quite common after antibiotic exposure, but we replenish our own ecosystems all the time because, like it or not, we frequently come into contact with other people's bacteria."
The big question, he says, is whether we're witnessing a global shift within our shared ecosystems. Is there a risk that the global populations of some species of bacteria are becoming more harmful?
"It's common sense that the most virulent, disease-causing bacteria are going to meet antibiotics more often, so it's common sense that they're also going to become more resistant. In this way, you expect virulence and antibiotic resistance to go together.
"The important question is whether we can reverse the trend. It's a similar debate to global warming. We simply don't know whether we're approaching some ecological tipping point, or understand the capacity of the system to recover."
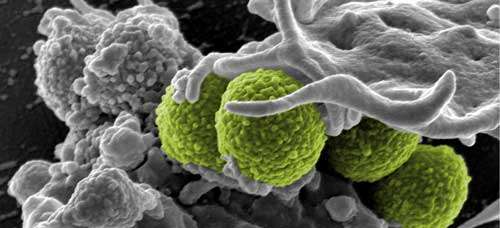
Professor Iredell's research group at Westmead Hospital in Sydney is trying to shed light on the problem by investigating the exchange of genes among bacteria. "It's all about competition," he says. "Bacteria are always fighting for advantage, and resistance to antibiotics is an obvious one."
Gene exchange between common gut bacteria like E. coli is mostly via specialised vehicles called plasmids, which normally live in bacteria and really only started to carry resistance genes after antibiotics became widely used. The same sort of ecological dynamics seems to operate, with bacteria having plasmid preferences and vice versa - just like bacteria and their mammalian hosts. The plasmid-bacteria relationship is one way in which virulence and resistance evolves together.
"In places where rivers and lakes contain antibiotics, you find a lot of resistance plasmids in E. coli in surface waters where people drink and bathe. It may be that resistance plasmids are now displacing the sensitive, diverse plasmids that have been there since mammals first appeared. In Beijing, Chicago, Sydney, Santiago, resistance plasmids look much the same, but antibiotic-susceptible ones seem more diverse. It's as though a cane toad has arrived in a rainforest and is displacing native frogs.
"Currently, if you come home from overseas with a resistant infection, we can treat the infection and kill the bacteria but we can't get rid of those resistance plasmids. They move into other bacteria and create a risk of later antibiotic failure if the plasmid hops back into a disease-causing strain - we've certainly seen this happen."
So are we approaching a tipping point where diverse native plasmids in bacteria like E. coli are being replaced by plasmids that are resistant to antibiotics? It's a question that worries Jon Iredell, because once those diverse antibiotic-sensitive plasmids are extinguished, they may be gone forever, and the ecological niches they occupied in bacteria may be occupied thereafter by resistance plasmids.
This in turn may mean that more virulent and resistant forms of bacteria - including those responsible for childhood diarrhoeal diseases all over the world - dominate the ecological niches that they occupy, such as the human gut.
"If you're not exposed to antibiotics, antibiotic-resistant plasmids and bacteria tend to be lost by simple dilution into local microbial populations," he says. "But in places where you don't meet sensitive bacteria and plasmids any more, you can't easily restore your own ecosystem."
He likens it to an arms race between two badly matched opponents. On the one side, humans spilling antibiotics into the ecosystem. On the other, bacteria with an infinite capacity for adaptation.
"You and I have probably got about a 5 per cent chance of having serious antibiotic resistance if we get, say, an E. coli infection at the moment. But our grandchildren - who knows? More worryingly, if resistance and virulence go together, the kind of E. coli we have now may be replaced by more resistant strains that are also more likely to cause disease."

















