The pathway to asthma winds through toll-like receptor 4
In a report that appears online in the journal Science, Dr. David Corry of Baylor College of Medicine and colleagues describe a molecule called toll-like receptor 4 that plays a key role in prompting the innate or immediate response that drives allergic disease and asthma.
Dr. David Corry compares the allergic response to a computer.
"The core of a computer is its CPU (central processing unit) or chip. We are looking for the chip that drives allergic disease," said the professor of medicine, chief of the section of immunology, allergy and rheumatology in Baylor College of Medicine's department of medicine and director of the Biology of Inflammation Center at BCM. In a report that appears online in the journal Science, he and colleagues at BCM describe an important component of that chip – a molecule called toll-like receptor 4 that plays a key role in prompting the innate or immediate response that drives allergic disease and asthma.
Asthma is part of a battle that takes place as the immune system marshals its forces to fight off an invading organism-or what mimics such invaders. The ensuing fight takes a significant toll on the human airway and lungs, often generating a violent and itself potentially deadly reaction – asthma.
In 2002, Corry and his colleagues found that proteinases, enzymes that chop up other proteins, are important in initiating the adaptive immune response that prompts generation of the critical T-cells and B-cells that populate the adaptive immune system. The adaptive immune system specifically targets allergens, and Corry knew that the more immediate innate immune system also played an important role in asthma and allergy.
"If you take many proteinases and give them to mice, they will induce an allergic disease that resembles asthma," he said.
With that key finding in the adaptive immune system, the researchers turned their attention to the puzzle presented by the innate immune system.
"What is the relationship between proteinases and asthma?" he said. Other work in the field pointed to another immune molecule called toll-like receptor 4 that was believed to play a role in activating T-helper type 2 (Th2) cells.
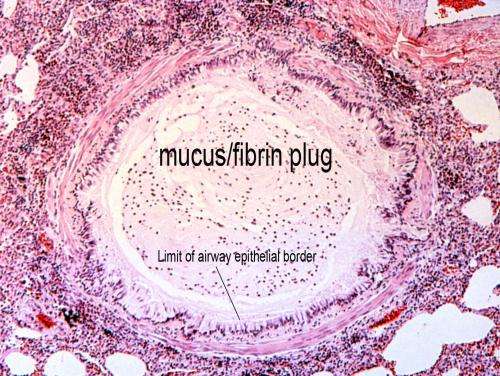
Instead, he and his colleagues found that the proteinases carve up a protein known as fibrinogen, leaving behind fragments that signal through the crucial toll-like receptor 4 to activate the cells of the innate immune system – the macrophages of the airway and airway epithelia.
"Toll-like receptor 4 is not required for the Th2 response itself," said Corry. "But, the Th2 response is proteinase dependent."
"When the macrophages are activated by fibrinogen cleavage products in culture, you get beautiful activation," said Corry.
In the airway, the same fibrinogen fragments that are part of the blood clotting process can cause clotting that is a barrier to breathing, said Corry.
In his studies, he used proteinase-producing fungi as the environmental trigger for asthma. Laboratory mice that lacked toll-like receptor 4 did not mount a robust allergic airway disease when challenged by proteinase, viable fungi or other triggers but did have a normal Th2 immunity.
"Why do our bodies do this?" said Corry. The answer is both simple and complicated. The system developed to allow organisms to survive infection with deadly organisms such as fungi. How it achieves that is complicated. In this "survival mode," the immune system generates symptoms that can themselves create disease.
Against the insidious onslaught of organisms such as fungi, which can kill if left unchecked, asthma may be a better alternative, said Corry.
"If you don't fight fungi off, they will get you," he said.
More information: "Cleavage of Fibrinogen by Proteinases Elicits Allergic Responses Through Toll-Like Receptor 4," by V.O. Millien et al Science, 2013.
















