Microbial restoration of the inflamed gut
A team led by gastroenterologists Sieglinde Angelberger and Walter Reinisch (Medical University Vienna) and microbiologists David Berry and Alexander Loy (University of Vienna) explored how a treatment called "fecal microbiota transplantation" can be used to support microbial recolonization of the gut of patients with chronic intestinal inflammation (ulcerative colitis). In this unusual alternative therapy the gut microbiota of healthy donors is transmitted to patients. The results of this pilot clinical study appear in the scientific journal American Journal of Gastroenterology.
About two million people in Europe suffer from chronic inflammatory bowel diseases, which are characterized by progressive tissue destruction and that often necessitate removal of sections of the intestine. The exact causes of Crohn's disease and ulcerative colitis, the most common forms of these diseases, are still largely unknown. In addition to genetic and environmental as well as lifestyle factors, a disturbed intestinal microbiota is responsible for triggering the disease. Complete recovery is often not possible. "If drug therapies fail, removal of parts of the inflamed intestine is currently the last treatment option," said Walter Reinisch, a gastroenterologist at the University Clinic for Internal Medicine III, Medical University of Vienna, and initiator of the study.
Fecal transplantation: an alternative therapy with a certain "yuck" factor
The idea of the transfer of fecal matter naturally causes some disgust. However, in many infectious and chronic diarrheas the intestinal microbiota is massively disrupted and it is therefore fecal transplantation can be used to restore the natural intestinal microbiota and thereby improve disease state. "Meta studies have shown that the controlled grafting of fecal transplantation from healthy donors is a safe and very effective treatment of acute diarrheal diseases caused by the pathogenic bacterium Clostridium difficile," said Sieglinde Angelberger, gastroenterologist at the University Clinic for Internal Medicine III of the Medical University of Vienna and author of the study: "this was the reason why we applied this therapy for the treatment of patients with chronic intestinal diseases."
Successive colonization by donor intestinal bacteria
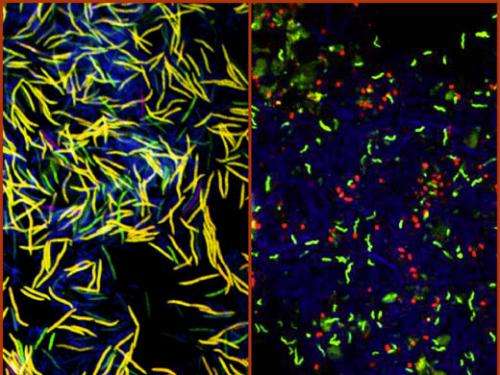
"So far, it has not been sufficiently tested whether and how successful fecal transplantation is for the permanent settlement of microbiota from a healthy donor to a patient," said Alexander Loy of the Department of Microbiology and Ecosystem Research, University of Vienna. "That is why we have followed the composition of the intestinal microbiota of patients using modern DNA sequencing methods over a period of up to three months after treatment."
The intestinal ecosystem of each individual patient reacted very differently to the fecal transplantation. Intestinal bacteria of the donors were detected in the patients, but at different times and in different frequencies. "Although we don't know the mechanisms yet, repopulation of the gut by bacteria appears to analogous to succession in a forest after it is damaged in a storm," said microbiologist David Berry: "pioneer species colonize the deforested area, in this case the inflamed intestine, and alter the ecosystem in a way that lets other species colonize and eventually a complex ecosystem can be restored."
More information: Temporal bacterial community dynamics vary among ulcerative colitis patients after fecal microbiota transplantation, By: Sieglinde Angelberger, Walter Reinisch, Athanasios Makristathis, Cornelia Lichtenberger, Clemens Dejaco, Pavol Papay, Gottfried Novacek, Michael Trauner, Alexander Loy and David Berry. In: American Journal of Gastroenteroloy (AJG), September 2013. www.nature.com/ajg/journal/vao … ull/ajg2013257a.html

















