3Qs: The effect of antibiotic resistant bacteria
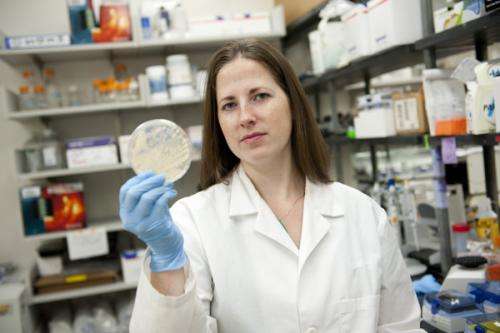
Last month, the Centers for Disease Control and Prevention released a report titled Antibiotic resistance threats in the United States, 2013, that served as a first-ever snapshot of the effect antibiotic resistant microbes have on human health. The report cited estimates that 2 million Americans become infected with resistant bacteria each year, 23,000of whom die from their infections. We asked Betsy Hirsch, an assistant professor in the Bouvé College of Health Sciences' Department of Pharmacy Practice, whose research currently focuses on treating a particular class of resistant bugs through combination therapies, to explain the report's significance.
What are antibiotic-resistant bacteria and why are they of increasing concern?
Antibiotic-resistant bacteria have evolved or acquired mechanisms that make them resistant to, generally speaking, multiple classes of antibiotics. The overuse or inappropriate use of antibiotics in both humans' health and agriculture can lead to the emergence and spread of antibiotic-resistant bacteria. The CDC report describes that a disturbing number—up to 50 percent—of all prescribed antibiotics are unnecessary or inappropriately prescribed.
Antibiotic-resistant bacteria are of increasing concern because the antibiotic pipeline is drying up. A significant amount of money and time go into the development of a new drug, and because antibiotics are often viewed as short-course therapies, this can mean low returns on investments. In addition, an unpredictable and often unattainable approval process for new antibiotics at the Food and Drug Administration has resulted in many companies abandoning research and development of new antibiotics. In fact, the FDA has only approved six new antibiotics in the past 10 years. As a result of this diminishing pipeline and the continuous evolution of bacteria, there may only be few, if any, effective antibiotics against infections caused by these resistant organisms.
What are the main findings of the CDC report and why is it getting so much attention?
This report is the first time the CDC has pooled all of its data on antibiotic resistance and concisely organized it all in one place. For the first time, it has prioritized bacteria into one of three "threat level" categories: urgent, serious, and concerning. For organisms within each of the threat levels, yearly estimates of infections and attributable deaths are given.
The document urges a call to action to combat this serious health threat. If steps are not immediately taken to halt the spread of antibiotic resistance, we are at risk of returning to the pre-antibiotic era. Without effective antibiotics, many modern medical advances, like organ transplants and cancer therapies, will no longer be possible since these patients are considerably more susceptible to infection.
Where does the health community go from here?
In the battle between men and microbes, we will never win, but there are some essential steps that can be taken to potentially limit the emergence of antibiotic resistance. First, raising awareness among the public that antibiotics can be harmful is critical; the CDC should be applauded for its efforts in releasing this report. Long-term solutions that may contribute to slowing the development and spread of antibiotic-resistant infections include infection control and prevention; increased monitoring and surveillance of bacterial resistance trends in the U.S.; improving antibiotic prescribing and use; and the development of new antibiotics.
In the short term, it will be imperative to identify antimicrobial combinations that are effective for antibiotic-resistant organisms, when few or no effective single-agent regimens exist. In particular, our lab is currently studying a specific type (Klebsiella pneumoniae carbapenemases [KPCs]) of carbapenem-resistant Enterobacteriaceae, which the CDC has placed in the highest threat level category. These organisms are resistant to most antibiotics on the market and nearly half of patients infected with this pathogen will die. We are studying the killing capacity of various combinations of antibiotics currently available on the market. Although KPC-producing bacteria may be resistant to these antibiotics when used alone, we are searching for synergistic combinations that effectively kill the bacteria when used together.


















